- Home
- News
- AngelBox
- About us
- Parent Support
- Borough Support
Winter is coming! See what support is available in your area
More features & information coming soon
- Health & Wellbeing Hub
- Get Involved
- Contact us
- Home
- News
- AngelBox
- About us
- Parent Support
- Borough Support
Winter is coming! See what support is available in your area
More features & information coming soon
- Health & Wellbeing Hub
- Get Involved
- Contact us
Your Health & Wellbeing Hub
Welcome to our Health & Wellbeing Hub your new comprehensive guide on how to access crucial NHS services when you or child is in most need.
Click on the relevant service to get more information
The NHS is here to SAVE YOU NOT FAIL YOU
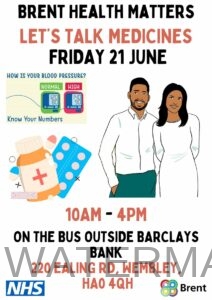
Our Health & Community Outreach 2024
We’re helping the NHS again this summer 2024 and this time it’s to raise awareness about several key diseases, viruses and their prevalence in society and how to avoid them. As well as key information and guidance on several health & wellbeing issues such as mental health, self care and how to even spot symptoms of cancer.
Our health & wellbeing hub is a convenient, easy read all in one page which highlights everything NHS & community.
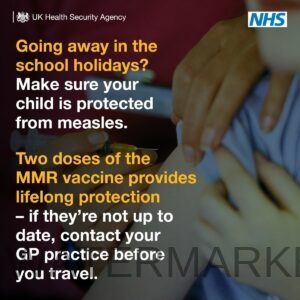
Our focus throughout the summer will be to promote the importance of early detection through the many ways to get a screening if your concerned about your health and discuss with parents about any barriers, concerns or experiences you have with regards to things like the MMR vaccine, the 6 in 1 baby jab and even how to protect yourself from common illness such as flu all the way to getting immunity from the rising cases of measles and whooping cough.
We’ve partnered with the North West London Integrated Care System to support their outreach to London residents about all the health & clinical services available to you right now and to also gauge your opinion on your recent experience of using a NHS service such as visiting your GP.
We will also place multilingual flyers in all our emergency relief packages which includes simple guides on how to access NHS services 24 hours a day, no matter the health emergency.
Measles, Mumps & Rubella (MMR)
These 3 infections spread easily between people and can lead to serious problems including meningitis, blindness and hearing loss.
If you’re pregnant, getting measles can cause premature birth, miscarriage or stillbirth. And getting rubella can cause serious problems for your baby such as damage to their sight and hearing.
2 doses of the MMR vaccine gives you long-term protection.
Getting vaccinated also helps protect people who cannot be vaccinated, such as unborn babies, newborn babies and anyone with a weakened immune system.
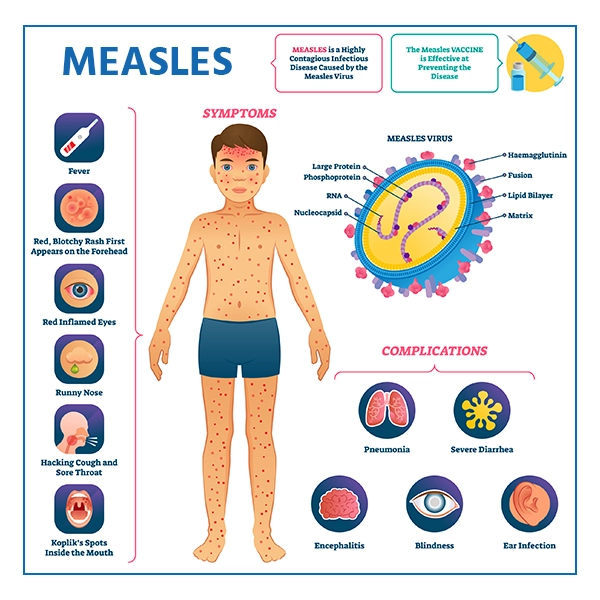
A brief about measles
Measles is an infection that spreads very easily and can cause serious problems in some people. Having the MMR vaccine is the best way to prevent it.
Measles usually starts with cold-like symptoms, followed by a rash a few days later. Some people may also get small spots in their mouth.
Cold-like symptoms
The first symptoms of measles include:
- a high temperature
- a runny or blocked nose
- sneezing
- a cough
- red, sore, watery eyes
Look out for
Small white spots may appear inside the cheeks and on the back of the lips a few days later. These spots usually last a few days.
The measles rash
A rash usually appears a few days after the cold-like symptoms.
The rash starts on the face and behind the ears before spreading to the rest of the body. The spots of the measles rash are sometimes raised and join together to form blotchy patches. They’re not usually itchy.
The rash looks brown or red on white skin. It may be harder to see on brown and black skin.

When to get help
Ask for an urgent GP appointment or get help from NHS 111 if:
- you think you or your child may have measles
- your child is under 1 year old and has come into contact with someone who has measles
- you’ve been in close contact with someone who has measles and you’re pregnant or have a weakened immune system
- you or your child have a high temperature that has not come down after taking paracetamol or ibuprofen
- you or your child have difficulty breathing – you may feel more short of breath than usual
- your baby or young child is not feeding well, or taking less feeds or fluids than usual
- you or your child are peeing less than usual (or your baby has fewer wet nappies)
- you or your child feels very unwell, or you’re worried something is seriously wrong
Measles can spread to others easily. Call your GP surgery before you go in. They may suggest talking over the phone.
You can also call 111 or get help from 111 online.


What to do at home once diagnosed
Measles usually starts to get better in about a week.
After seeing a GP, there are things you can do to help ease the symptoms and reduce the risk of spreading the infection.
It can help to:
- rest and drink plenty fluids, such as water, to avoid dehydration
- take paracetamol or ibuprofen for a high temperature
- give your child paracetamol or ibuprofen if they’re distressed or uncomfortable – check the packaging or leaflet to make sure the medicine is suitable for your child, or speak to a pharmacist or GP if you’re not sure
- use cotton wool soaked in warm water to gently remove any crusts from your or your child’s eyes
IMPORTANT ADVICE
Stay off nursery, school or work for at least 4 days from when the rash first appears.
Also try to avoid close contact with babies and anyone who is pregnant or has a weakened immune system.
IF YOUR NOT SURE ABOUT YOUR SYMPTOMS IT’S BEST TO CALL YOUR GP OR DIAL 111.
CALL 999 IF
You or your child has measles and:
- have a seizure (fit)
- severe difficulty breathing – you’re gasping, choking or not able to get words out (babies may make grunting noises or their stomach may suck under their ribcage)
- are unable to stay awake – cannot keep their eyes open for more than a few seconds
- suddenly become confused – your child may be very unsettled, behaving differently, or crying non-stop
- your child is limp, floppy or not responding normally – their head may fall to the side, backwards or forwards, or they may find it difficult to lift their head and focus on your face
- a rash that does not fade when you press a glass against it
- a stiff neck, or find light uncomfortable or painful
Complications of measles IF IGNORED
Measles can lead to serious problems if it spreads to other parts of the body, such as the lungs or brain.
Problems that can be caused by measles include:
- pneumonia
- meningitis
- blindness
- seizures (fits)
These problems are rare, but some people are more at risk. This includes babies and people with weakened immune systems.
Measles in pregnancy
If you get measles when you’re pregnant, it could harm your baby.
It can cause:
- miscarriage or stillbirth
- premature birth (before the 37th week of pregnancy)
- your baby having a low birthweight
It’s important to get medical advice if you’re pregnant and have been in close contact with someone who has measles.
A brief about Mumps
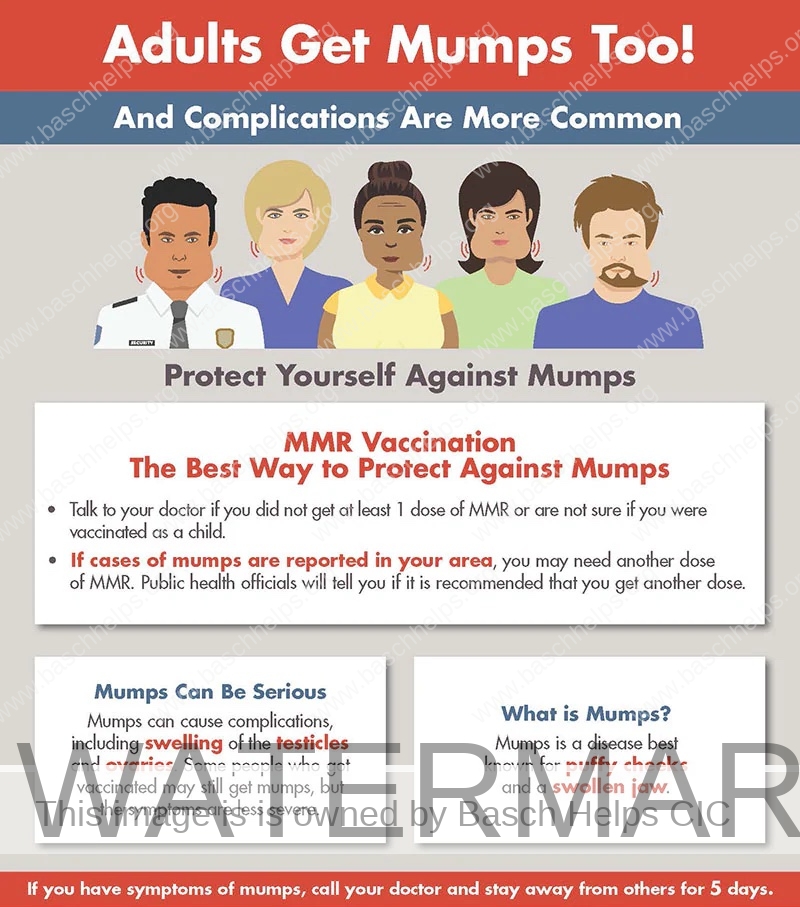
Mumps is a contagious viral infection that used to be common in children before the introduction of the MMR vaccine.
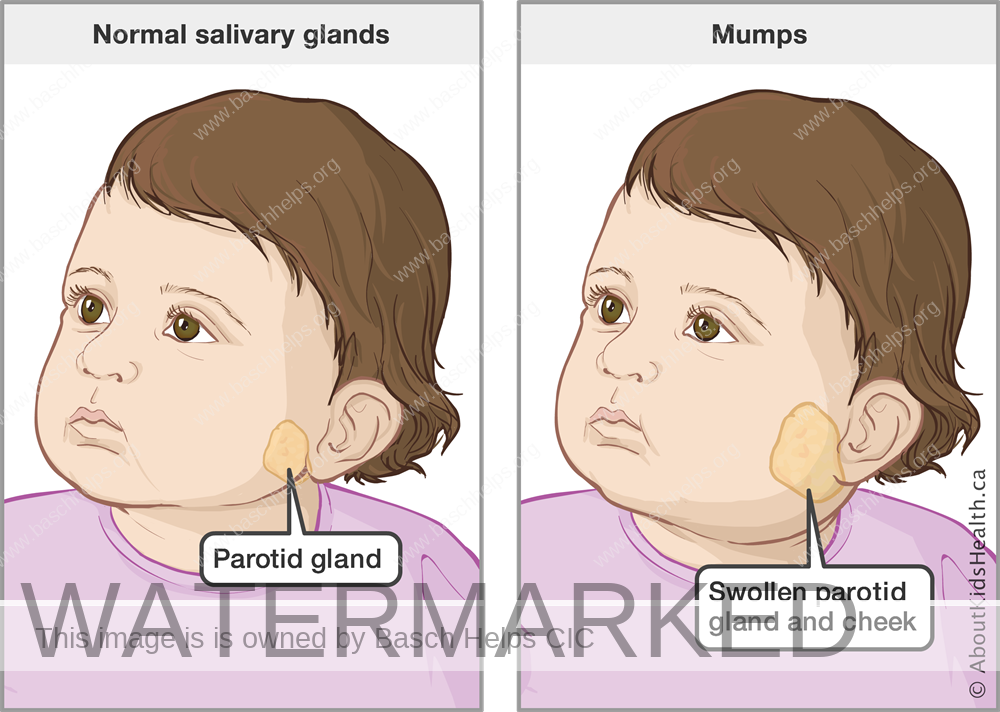
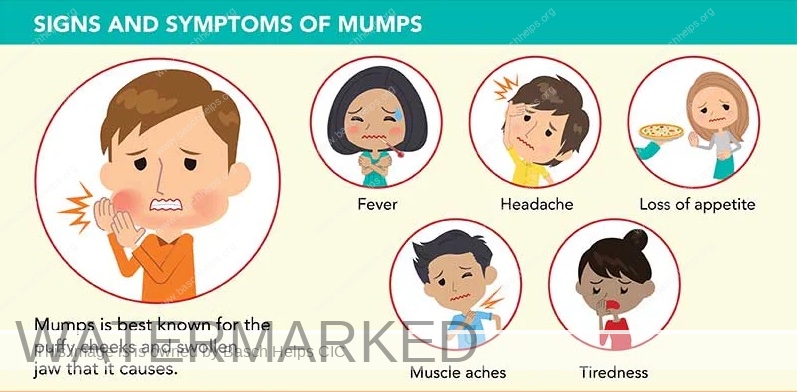
Mumps is most recognisable by the painful swellings in the side of the face under the ears (the parotid glands), giving a person with mumps a distinctive “hamster face” appearance.
Other symptoms of mumps include headaches, joint pain, and a high temperature, which may develop a few days before the swelling of the parotid glands.

Look out for
The symptoms of mumps usually develop 12 to 25 days after becoming infected with the mumps virus (this delay is known as the incubation period). The average incubation period is around 17 days.
Swelling of the parotid glands is the most common symptom of mumps. The parotid glands are a pair of glands responsible for producing saliva. They’re located in either side of your face, just below your ears.
Both glands are usually affected by the swelling, although sometimes only one gland is affected. The swelling can cause pain, tenderness and difficulty with swallowing.
More general symptoms often develop a few days before the parotid glands swell. These can include:
- headache
- joint pain
- feeling sick
- dry mouth
- mild abdominal pain
- feeling tired
- loss of appetite
- a high temperature
When to get help
If you suspect mumps, it’s important to call your GP.
While the infection isn’t usually serious, mumps has similar symptoms to other, more serious infections, such as glandular fever and tonsillitis. It’s always best to visit your GP so they can confirm (or rule out) a diagnosis of mumps.
It’s also important to let your GP know in advance if you’re coming to the surgery so they can take any necessary precautions to avoid the spread of infection.
What to do at home once diagnosed
Treatment for mumps is focused on relieving symptoms until your body’s immune system fights off the infection. There are currently no medicines to treat the mumps virus.
The infection usually passes within a week or two.
In the meantime, the measures below may help.
- get plenty of bed rest until your symptoms have passed
- take over-the-counter painkillers, such as ibuprofen or paracetamol, to relieve any pain (children aged 16 or under should not be given aspirin)
- drink plenty of fluids, but avoid acidic drinks such as fruit juice as these can irritate your parotid glands; water is usually the best fluid to drink
- apply a warm or cool compress to your swollen glands to help reduce any pain
- eat foods that don’t require a lot of chewing, such as soup, mashed potatoes and scrambled eggs
IMPORTANT ADVICE
-
stay away from school, college or work until 5 days after you first developed symptoms
-
wash your hands regularly, using soap and water
-
always use a tissue to cover your mouth and nose when you cough and sneeze, and throw the tissue in a bin immediately afterwards
A brief about rubella (german measles)
Rubella (german measles) is a rare illness that causes a spotty rash. It usually gets better in about a week, but it can be serious if you get it when you’re pregnant.
The main symptom of rubella is a spotty rash that starts on the face or behind the ears and spreads to the neck and body.
The rash takes 2 to 3 weeks to appear after getting rubella.
Rubella can also cause:
- aching fingers, wrists or knees
- a high temperature
- coughs
- sneezing and a runny nose
- headaches
- a sore throat
- sore, red eyes
When to get help
If you suspect rubella, it’s important to call your GP.
It’s also important to let your GP know in advance if you’re coming to the surgery so they can take any necessary precautions to avoid the spread of infection.
Call your midwife, maternity unit, or GP immediately if:
You’re pregnant and either:
- you have a new rash
- you’ve been in close contact with someone who has rubella

What to do at home once diagnosed
Rubella usually gets better in about a week.
After getting advice from a GP, you or your child should:
- get plenty of rest
- drink lots of fluids, like water or squash
- take paracetamol or ibuprofen if you’re uncomfortable – do not give aspirin to children under 16
Rubella is very rare in pregnancy. But if you get it when you’re pregnant, rubella could harm your baby.
It can cause:
- loss of the baby (miscarriage)
- serious problems after the baby is born – such as problems with their sight, hearing, heart, or brain
The risk is highest if you get rubella early in pregnancy.
There’s not thought to be a risk to your baby if you get rubella after week 20 of your pregnancy.
What the MMR vaccine is for
The MMR vaccine protects against:
These 3 infections spread easily between people and can lead to serious problems including meningitis, blindness and hearing loss.
If you’re pregnant, getting measles can cause premature birth, miscarriage or still birth. And getting rubella can cause serious problems for your baby such as damage to their sight and hearing.
2 doses of the MMR vaccine gives you long-term protection.
Getting vaccinated also helps protect people who cannot be vaccinated, such as unborn babies, newborn babies and anyone with a weakened immune system.
MMR vaccination for children under 10
The MMR vaccine is recommended for all babies and young children, but older children and adults can have it if they were not vaccinated when they were younger.
Babies and young children
Babies and young children are given 2 doses of the MMR vaccine as part of the NHS vaccination schedule.
They’re given a dose at:
- 1 year old
- 3 years 4 months old
Babies between 6 and 12 months can have an extra dose of the MMR vaccine before this if they need it to protect them if:
- they’re travelling abroad to an area with a lot of measles
- they’ve been close to someone with measles
- there’s an outbreak of measles

Teenageers & Adults are eligible too!
The MMR vaccine can be given at any age.
Speak to a GP about getting vaccinated if you did not have it as a child, you only had 1 dose or you’re not sure if you’ve been fully vaccinated.
It’s especially important to make sure you’re vaccinated if:
- you’re a child, teenager or young adult
- you could become pregnant
- you’re travelling to, or living in, a country where there is a higher risk of getting measles, mumps or rubella
- you’re a healthcare worker
- you were born between 1970 and 1990 (as you may not have been vaccinated against all 3 infections)
Your GP surgery should be able to tell you which vaccinations you’ve already had.
MMR Vaccine Ingredients
There are 2 types of MMR vaccine in the UK. You can check the ingredients in the patient leaflets:
- MMRVaXPro MMR vaccine patient leaflet (Electronic Medicines Compendium website)
- Priorix MMR vaccine patient leaflet (Electronic Medicines Compendium website; PDF only, 179KB)
The MMR VaxPro vaccine contains a small amount of gelatine from pigs (porcine gelatine). Speak to the person vaccinating your child if you want your child to have the Priorix MMR vaccine instead.

How to get the MMR vaccine
Your GP surgery will usually contact you about your child’s MMR vaccinations. This will usually be by letter, text message, phone call or email.
Older children who missed being vaccinated when they were younger may also be able to get the MMR vaccine through their school.
If you need the MMR vaccine for your work, you should be able to get it through your employer’s occupational health service.
NHS Start For Life
Better Health – Start for Life. Is a website for trusted NHS advice and guidance to help you have a healthy and happy baby during pregnancy, birth and parenthood.
What is NHS Start For Life
Your baby’s brain is making a million new connections every second, making the first two years so important for their healthy development.That means building strong connections during this period of your baby’s life lays the groundwork for their future well-being and mental health.
For the latest advice on how best to build your relationship with your baby, you can find support and free resources, including tips and learning materials, at the Start for Life Hub.

The NHS Healthy Start Scheme
If you’re more than 10 weeks pregnant or have a child under 4, you may be entitled to get help to buy healthy food and milk.
What is the NHS Healthy Start Scheme
If you’re more than 10 weeks pregnant or have a child under 4, you may be entitled to get help to buy healthy food and milk.
If you’re eligible, you’ll be sent a Healthy Start card with money on it that you can use in some UK shops. Your card is reloaded every 4 weeks.
You can use your card to buy:
- plain liquid cow’s milk
- fresh, frozen, and tinned fruit and vegetables
- fresh, dried, and tinned pulses
- infant formula milk based on cow’s milk
You can also use your card to collect:
- Healthy Start vitamins – these support you during pregnancy and breastfeeding
- vitamin drops for babies and young children – these are suitable from birth to 4 years old
Find out more
Official Healthy Start Website
Family Hubs
Family Hubs ensure families with children aged 0-19 can access integrated early help to overcome difficulties and build stronger relationships.
GP Services & Registration
This section is about GP services available locally to you, including how to find and register with a local GP and how to book an appointment.
GP Services
What is a GP? General practitioners (GPs) treat all common medical conditions and refer patients to hospitals and other medical services for urgent and specialist treatment.
A GP Practice has a wider team that promotes, prevents and offers treatment. Who care for people with chronic illness and long-term conditions, aiming to keep them well and in their own homes.
This section covers everything about GP services, including how to find and register with a local GP and how to book an appointment.
How to register with a GP surgery
You don’t need anything to register with a GP surgery
Anyone in London can register with a GP surgery. It’s free to register.
You do not need proof of address or immigration status, ID or an NHS number.
You might be able to register with a GP surgery that’s not in the area you live. Find out about registering with a GP surgery out of your area
GP surgeries are usually the first contact if you have a health problem. They can treat many conditions and give health advice. They can also refer you to other NHS services.

How to register with a GP surgery
Find a GP that suits what you need.
Some GP surgeries offer more services than others. You can look up GP surgeries to see what they offer and how they compare.
Because of coronavirus (COVID-19), try to avoid going into a GP surgery to register.
You can:
- check the GP surgery website to see if you can register online
- call or email the GP surgery and ask to be registered as a patient
You can download a GMS1 registration form on GOV.UK if you’re asked to complete one. (External Link)
You do not need proof of ID to register with a GP, but it might help if you have one or more of the following:
- passport
- birth certificate
- HC2 certificate
- rough sleepers’ identity badge
- hostel or accommodation registration or mail forwarding letter
If you’re homeless, you can give a temporary address, such as a friend’s address, a day centre or the GP surgery address.
Changing your GP surgery is simple
You can change your GP surgery if you need to.
This might be because:
- you have moved
- you have had problems with your current practice
- you were removed from the patient list
You should tell the GP surgery if you change address or move out of the area.

GP appointments and bookings
How to book, change or cancel an appointment at your GP
You should be able to book or change an appointment at your GP surgery:
- online, find out more about how to start using online services
- by phone
- in person, by going into the surgery and talking to the receptionist
In some GP surgeries, you may also be able to have a consultation online or over the phone. Speak to your GP surgery for more information about online and phone consultations.
Call your GP surgery if you need an urgent appointment. If your GP surgery is closed, a recorded message will tell you who to contact.
Find your GP surgery
Booking, changing and cancelling appointments online
If you are registered with a GP surgery, you can use their online services to book, check or cancel appointments with a GP, nurse, or other healthcare professional.
If you have already signed up to online services, log in to your usual service provider and book one of the available appointments.
To change an appointment online, you will need to cancel the appointment you already have and book a new one.
Information:
Read more about how to start using online services, if you are not signed up to them already.
Pharmacies: Guidance & Information (London)
Find out how pharmacists can help with medicine and medical advice, and find your nearest pharmacy.
Pharmacies
Your local pharmacist is more than somebody who dispenses medicine their actually fully qualified healthcare professionals.
As qualified healthcare professionals, they can offer clinical advice and over-the-counter medicines for a range of minor illnesses, such as coughs, colds, sore throats, tummy trouble and aches and pains.
If symptoms suggest it’s something more serious, pharmacists have the right training to make sure you get the help you need. For example they will tell you if you need to see a GP, nurse or other healthcare professional.
All pharmacists train for 5 years in the use of medicines. They are also trained in managing minor illnesses and providing health and wellbeing advice.
Many pharmacies are open until late and at weekends. You do not need an appointment.
Most pharmacies have a private consultation room where you can discuss issues with pharmacy staff without being overheard.
Find your local pharmacy
Finding a pharmacy is simple. Use the free NHS Pharmacy directory by entering your town or post code on their website and a list of the nearest pharmacies will appear with closing times and address.

Help with minor health concerns
Pharmacies can give treatment advice about a range of common conditions and minor injuries, such as:
- aches and pains
- sore throat
- coughs
- colds
- flu
- earache
- cystitis
- skin rashes
- teething
- red eye
If you want to buy an over-the-counter medicine, the pharmacist and their team can help you choose.
Antibiotics will not be available over the counter to treat minor conditions.
New Medicine Service
If you’re prescribed a medicine to treat a long-term condition for the first time, you may be able to get extra help and advice about your medicine from your local pharmacist through a free scheme called the New Medicine Service (NMS).
People often have problems when they start a new medicine. As part of the scheme, the pharmacist will support you over several weeks to use the medicine safely and to best effect.
The New Medicine Service is available at pharmacies to give you extra help and advice if you’re just starting on a new medicine for one of the following conditions:
- asthma
- chronic obstructive pulmonary disease (COPD)
- type 2 diabetes
- high blood pressure
- people who have been given a new blood-thinning medicine

Help with your medicine
Pharmacists can answer your questions on prescription and over-the-counter medicines.
All pharmacies provide the following services:
- dispensing of NHS prescriptions
- access to the repeat prescription service (with agreement from your GP)
- an emergency supply of medicine, subject to the decision of the
- pharmacist (you may need to pay for an emergency supply)
- non-prescription medicines like paracetamol
- disposal of unwanted or out-of-date medicines
- advice on treating minor health concerns and healthy living
Pharmacy technicians can help with things like:
- inhaler technique
- how to take a medicine safely
- helping you understand the correct dose of a new medicine and how often
- you need to take it
Some pharmacies will deliver your prescription medicines to you, but you may need to pay for this service. You can use the Find a pharmacy service and check the treatments and services page of the pharmacy profile to see if they offer this service.
Repeat Prescriptions
Repeat prescriptions can be issued in 2 different ways:
- You order the prescription to be approved by a GP each time you need a refill.
- You order the prescription once and a GP approves a series of refills for you. They are sent to the pharmacy automatically, so you do not need to order them each time. This is called electronic repeat dispensing. The GP surgery or pharmacy will let you know when you need to re-order your prescription.
In both cases, you can:
- choose a specific pharmacy (nominated pharmacy) to collect your prescriptions from each time – call or contact the pharmacy online a few days before you run out of medicine to check your prescription is ready to collect
- decide each time you’re given a prescription where to collect it – you’ll be given a paper copy with a barcode to take to any pharmacy in England, or the pharmacy can find your prescription using your NHS number
As part of the repeat prescription service, the pharmacist will ask if you’re having any problems or side effects with your medicines and, where appropriate, they can discuss this with you and your GP.

NHS App: Guidance & Information
Download the NHS App or open the NHS website up and login to access a range of NHS services online.

The NHS App
The NHS App has been developed by the NHS to help people in England get more information about their health and care – and more control of how they use NHS services.
Available to download on all iOS and Android devices, it allows you to book appointments at your GP surgery, manage repeat prescriptions, view your GP medical records, set organ donation preferences and much more. New functions and services will also be added in the coming months.

What can I do on the NHS App?
You’ll need to provide extra proof of who you are to get full access to your NHS account. Once you have full access, you can:
- order repeat prescriptions – see your available medicines, request a new repeat prescription and choose a pharmacy for your prescriptions to be sent to
- book appointments – search for, book and cancel appointments at your GP surgery, and see details of your upcoming and past appointments
- view your health record – securely access your GP health record, to see information like your allergies and your current and past medicines. If your GP has given you access to your detailed medical record, you can also see information like test results and details of your consultations
- get your NHS COVID Pass – view and download your COVID Pass for travel abroad. There are also other ways to get your NHS COVID Pass
- register your organ donation decision – choose to donate some or all of your organs and check your registered decision
find out how the NHS uses your data – choose if data from your health records is shared for research and planning
view your NHS number – find out what your NHS number is

Mental Health Support: Guidance & Information (London Only)
Find information and support for your mental health.
NHS Mental Health Services
Your mental health is important
As many as one in four people will experience some form of mental illness at some point in their lives. Mental health problems range from reactions to normal life events, such as bereavement, relationship breakdowns and depression, to more complex conditions such as schizophrenia.
If you are experiencing an issue with your mental health it is important to know that you are not alone and that there is plenty of support available to help improve your mental well-being.
The first place to get help is your GP. They are best placed to offer you initial advice on how to deal with your symptoms and talk to you about available treatments and support services in your area.
GET HELP TODAY
If you are already a service user and you have a mental health crisis during normal office hours (Monday to Friday, 9am to 5pm), your first point of contact should be the person that you usually see (your care coordinator, or named lead professional).
If you, or a friend or relative are experiencing mental health problems for the first time and need emergency treatment or advice during office hours, then you should contact your general practitioner (GP). They will be able to refer you to the most appropriate mental health service in your area.
In an emergency, if your GP surgery is closed, you should call your local Single Point of Access (SPA):
If you live in Brent, Harrow, Hillingdon, Kensington & Chelsea or Westminster call 0800 023 4650
If you live in Ealing, Hammersmith and Fulham or Hounslow call 0800 328 444.
Trained mental health advisors and clinicians are available to provide help and advice in a crisis 24 hours a day, 7 days a week, 365 days a year.

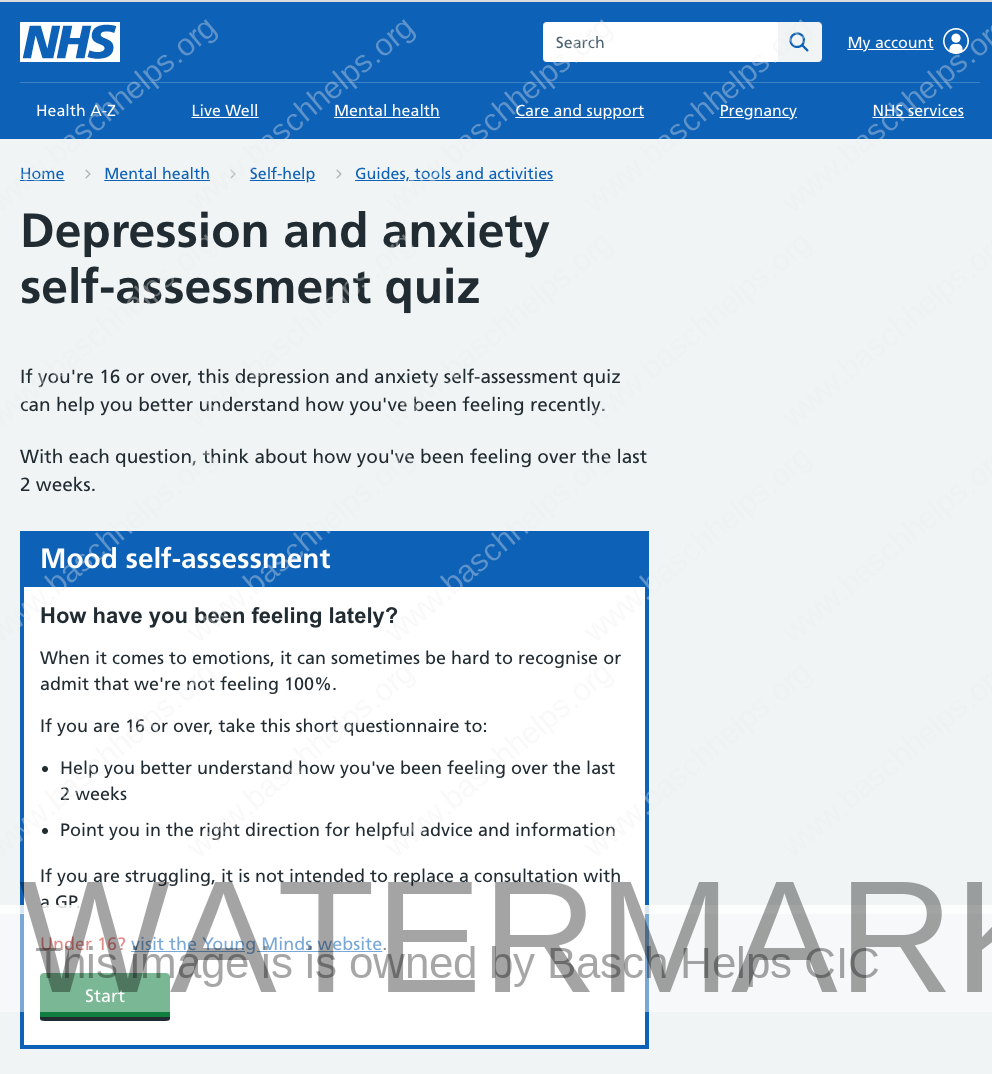
NHS Mood Self-Assessment Tool
This quiz uses questions that GPs often use to assess whether someone is anxious or depressed. It also includes links to useful information and advice on mental wellbeing.
There are 18 questions altogether. With each one, you’ll need to think about how you’ve been feeling over the past 2 weeks.
You can monitor any ups and downs of your mood by revisiting this self-assessment quiz at any time.
Coping with mental health
Right now, it has never been more important for each of us to think and talk more about mental health and wellbeing, and to seek support when needed.
There is help and support available for whatever you are going through:
We offer wellbeing and psychological support, if you are feeling low, anxious or depressed from our talking therapies services. You can refer yourself or speak to your GP or another healthcare professional for a referral. For more information visit www.nhstalk2us.org
Across London, there is also a range of practical advice and support available from Every Mind Matters, Good Thinking, and Thrive LDN.
If you feel more comfortable talking to someone you don’t know, you can use one of the following helplines:
Samaritans are here when life is difficult. They won’t judge you or tell you what to do, they’re here to listen so you don’t have to face it alone. Call the free, 24-hour listening service on 116 123 or email jo@samaritans.org.
Shout is the UK’s first 24/7 text messaging service for anyone in crisis. Text Shout at any time to 85258 to start a conversation with a trained volunteer.
Mental health support for young children
CAMHS stands for Child and Adolescent Mental Health Services and treats young people with emotional, behavioural or mental health difficulties.
CAMHS support covers depression, problems with food, self-harm, abuse, violence or anger, bipolar, schizophrenia and anxiety, to name a few.
In North West London CAMHS services are provided by the Central and North West London NHS Foundation Trust and the West London NHS Trust.
If you need mental health help or advice for a child or young person in an emergency and their GP surgery is closed, you should call your local Single Point of Access (SPA):
If you live in Brent, Harrow, Hillingdon, Kensington & Chelsea or Westminster call 0800 023 4650
If you live in Ealing, Hammersmith and Fulham or Hounslow call 0800 328 444 and choose option 2.
Trained mental health advisors and clinicians are available to provide help and advice in a crisis 24 hours a day, 7 days a week, 365 days a year.
Kooth
Kooth is an online mental wellbeing community offering free, safe and anonymous support for younger people aged 11-25, living in Brent, Harrow, Hillingdon, Kensington & Chelsea, Westminster, Ealing, Hammersmith & Fulham and Hounslow.
If you’re feeling sad, anxious, or finding life hard, Kooth is available to support you kooth.com.

Self-Care: Guidance & Information
Find tips, guides, tools and activities to support and improve mental health.
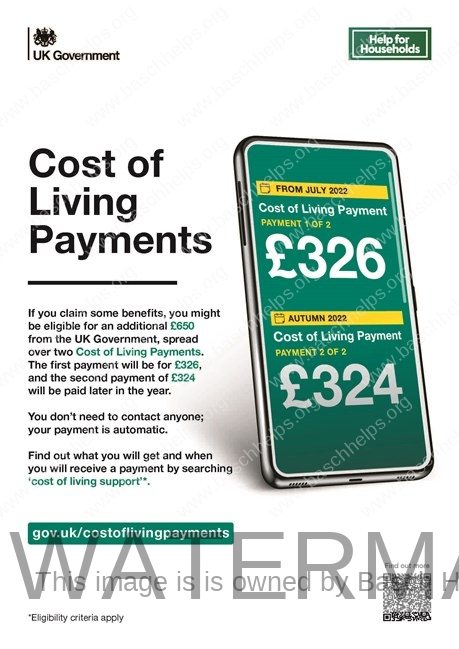
Winter Healthy Living & Staying Well
The NHS has provided advice and recommendations about healthy living, including eating a balanced diet, healthy weight, exercise, quitting smoking and drinking less alcohol.
Cold weather can make some health problems worse and even lead to serious complications, especially if you’re 65 or older, or if you have a long-term health condition.
- people aged 65 and older
- babies and children under the age of 5
- people on a low income (so cannot afford heating)
- people who have a long-term health condition
- people with a disability
- pregnant women
- people who have a mental health condition
How to stay warm
Keeping warm over the winter months can help to prevent colds, flu and more serious health problems such as heart attacks, strokes, pneumonia and depression.
Heat your home to a temperature that’s comfortable for you. If you can, this should be at least 18°C in the rooms that you regularly use, such as your living room and bedroom. This is particularly important if you have a health condition. It’s best to keep your bedroom windows closed at night.
Check your heating and cooking appliances are safe. Contact a Gas Safe registered engineer to make sure they’re working properly. You can find an engineer from the Gas Safe Register website.
Make sure you’re getting all the help that you’re entitled to. There are grants, benefits and advice available to make your home more energy efficient, improve your heating or help with bills.
Find out more about ways to save energy in your home from GOV.UK, or call the government helpline on 0800 444 202.
You can also find out more from GOV.UK about benefits and financial support if you’re on a low income.
Check out our Cost of Living Hub
For more information and guidance on how local boroughs and the government can financially support you through these difficult times check out our Cost of Living Hub.

How winter can affect you
If you’re worried about your health, don’t delay – help us help you get the care you need this winter. Winter conditions can be bad for our health, especially for people aged 65 or older, and people with long-term conditions such as heart or kidney disease, COPD, bronchitis, emphysema, asthma or diabetes.
Being cold can raise the risk of increased blood pressure, heart attacks and strokes.
The cold and damp weather, ice, snow and high winds can all aggravate any existing health problems and make us more vulnerable to respiratory winter illnesses. But there are lots of things you can do to stay well this winter.
Some videos to keep you active & warm this winter
Exercise your way to better health
Many of us are having to spend more time at home which can make it harder to keep active. It’s important to continue to do what you can to help with your physical and mental health. There’s strong evidence that people who are active have a lower risk of heart disease, stroke, type 2 diabetes, some cancers, depression and dementia. Regular exercise can also reduce the risk of falling and can be beneficial for recovery if you do get ill. Try to reduce the amount of time you spend sitting down during the day.
Break up your time spent being inactive by walking around your home or standing up from your chair during TV advert breaks or when you’re on the phone. There are many activities you could do at home, such as walking up and down stairs, dancing, gardening, housework, or taking part in online fitness classes. It doesn’t matter what you do, as long as it’s something you enjoy and keeps you moving. Don’t do anything that doesn’t feel comfortable and trust your instincts about your own limits. Stop if you are feeling any pain or lightheaded and stay hydrated.
For tips on keeping active go to www.nhs.uk/keepactive or www.ageuk.org.uk


Getting a good nights sleep
Reasons why you might feel tired and advice about what you can do to prevent tiredness.
Feeling exhausted is so common that it has its own acronym, TATT, which stands for “tired all the time”.
We all feel tired from time to time. The reasons are usually obvious and include:
- too many late nights
- long hours spent at work
- a baby keeping you up at night
But tiredness or exhaustion that goes on for a long time is not normal. It can affect your ability to get on and enjoy your life.
Unexplained tiredness is one of the most common reasons for people to see their GP.
Ways to get a better sleep
- Make sure that your bed and bedroom are comfortable – not too hot, not too cold, not too noisy.
- Make sure that your mattress supports you properly. If it’s too firm, your hips and shoulders are under pressure. If it’s too soft, your body sags which is bad for your back. Generally, you should replace your mattress every 10 years to get the best support and comfort.
- Get some exercise. Don’t overdo it, but try some regular swimming or walking. The best time to exercise is in the daytime – particularly late afternoon or early evening. Later than this can disturb your sleep.
- Take some time to relax properly before going to bed. Some people find aromatherapy helpful.
- If something is troubling you and there is nothing you can do about it right away, try writing it down before going to bed and then tell yourself to deal with it tomorrow.
- If you can’t sleep, get up and do something relaxing. Read, watch television or listen to quiet music. After a while, you should feel tired enough to go to bed again.
Don’ts
- Don’t go without sleep for a long time. Go to bed when you feel tired and stick to a routine of getting up at the same time every day, whether you still feel tired or not.
- Caffeine hangs around in your body for many hours after your last drink of tea or coffee. There are now many fizzy drinks, and even mints, that contain a lot of caffeine. Stop drinking tea or coffee by mid-afternoon. If you want a hot drink in the evening, try something milky or herbal (but check there’s no caffeine in it).
- Don’t drink a lot of alcohol. It may help you fall asleep, but you will almost certainly wake up during the night.
- Don’t eat or drink a lot late at night. Try to have your supper early in the evening rather than late.
- If you’ve had a bad night, don’t sleep in the next day – it will make it harder to get off to sleep the following night.
- Don’t use slimming pills – many of these will keep you awake.
- Don’t use street drugs like Ecstasy, cocaine and amphetamines – they are stimulants, and like caffeine, will tend to keep you awake.
If you try these tips and you still can’t sleep, go and see your doctor.
You can talk over any problems that may be interfering with your sleep. Your doctor can check that your sleeplessness is not due to a physical illness, a prescribed medicine, or emotional problems. There is evidence that cognitive behavioural therapy can be helpful if you haven’t been sleeping well for some time.

Eat well
Information and guidance about eating a healthy, balanced diet.
Eating a healthy, balanced diet is an important part of maintaining good health, and can help you feel your best.
This means eating a wide variety of foods in the right proportions, and consuming the right amount of food and drink to achieve and maintain a healthy body weight.
This page covers healthy eating advice for the general population.
People with special dietary needs or a medical condition should ask their doctor or a registered dietitian for advice.
Eating a balanced diet
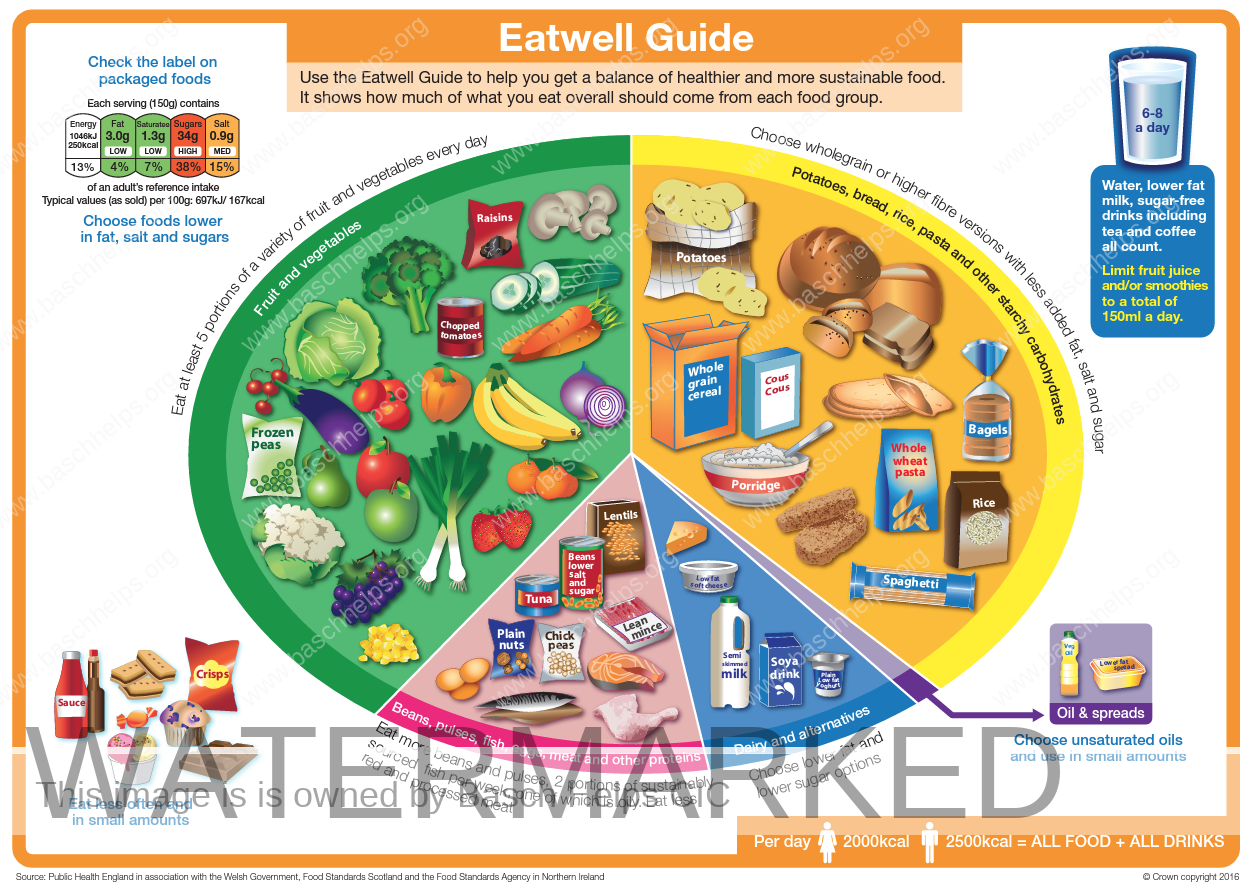
The Eatwell Guide shows that to have a healthy, balanced diet, people should try to:
- eat at least 5 portions of a variety of fruit and vegetables every day (see 5 A Day)
- base meals on higher fibre starchy foods like potatoes, bread, rice or pasta
- have some dairy or dairy alternatives (such as soya drinks)
- eat some beans, pulses, fish, eggs, meat and other protein
- choose unsaturated oils and spreads, and eat them in small amounts
- drink plenty of fluids (at least 6 to 8 glasses a day)
If you’re having foods and drinks that are high in fat, salt and sugar, have these less often and in small amounts.
Try to choose a variety of different foods from the 5 main food groups to get a wide range of nutrients.
Most people in the UK eat and drink too many calories, too much saturated fat, sugar and salt, and not enough fruit, vegetables, oily fish or fibre.
The Eatwell Guide does not apply to children under the age of 2 because they have different nutritional needs.
Between the ages of 2 and 5 years, children should gradually move to eating the same foods as the rest of the family in the proportions shown in the Eatwell Guide.
Fruit and vegetables: are you getting your 5 A Day?
Fruit and vegetables are a good source of vitamins and minerals and fibre, and should make up just over a third of the food you eat each day.
It’s recommended that you eat at least 5 portions of a variety of fruit and vegetables every day. They can be fresh, frozen, canned, dried or juiced.
There’s evidence that people who eat at least 5 portions of fruit and vegetables a day have a lower risk of heart disease, stroke and some cancers.
Eating 5 portions is not as hard as it sounds.
A portion is:
- 80g of fresh, canned or frozen fruit and vegetables
- 30g of dried fruit – which should be kept to mealtimes
- 150ml glass of fruit juice or smoothie – but do not have more than 1
- portion a day as these drinks are sugary and can damage teeth
Just 1 apple, banana, pear or similar-sized fruit is 1 portion each.
A slice of pineapple or melon is also 1 portion, and 3 heaped tablespoons of vegetables is another portion.
Adding a tablespoon of dried fruit, such as raisins, to your morning cereal is an easy way to get 1 portion.
You could also swap your mid-morning biscuit for a banana, and add a side salad to your lunch.
In the evening, have a portion of vegetables with dinner and fresh fruit with plain, lower fat yoghurt for dessert to reach your 5 A Day.
Find out more about what counts towards your 5 A Day

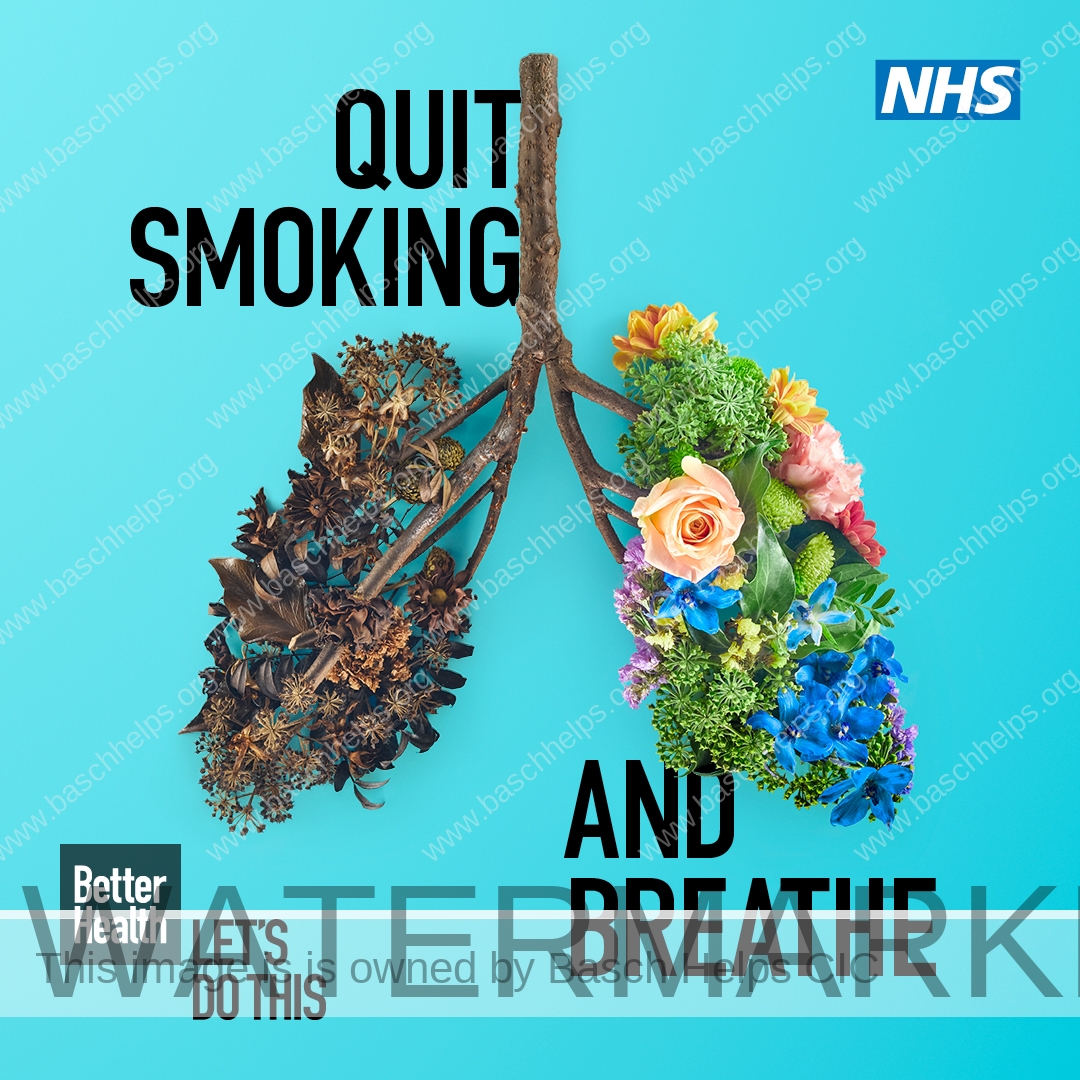
Quit smoking
Protecting your baby from tobacco smoke is one of the best things you can do to give your child a healthy start in life. It can be difficult to stop smoking, but it’s never too late to quit.
Every cigarette you smoke contains over 4,000 chemicals, so smoking when you are pregnant harms your unborn baby. Cigarettes can restrict the essential oxygen supply to your baby. As a result, their heart must beat harder every time you smoke.
Stopping smoking will help both you and your baby immediately. Harmful gases, such as carbon monoxide, and other damaging chemicals will clear from your body. When you stop smoking:
- you will reduce the risk of complications in pregnancy and birth
- you are more likely to have a healthier pregnancy and a healthier baby
- you will reduce the risk of stillbirth
- your baby is less likely to be born too early and have to face the breathing, feeding and health problems that often go with being premature
- your baby is less likely to be born with a low birth weight. Babies of smokers are, on average, 200g (about 8oz) lighter than other babies, which can cause problems during and after labour. For example, they are more likely to have problems keeping warm and are more likely to get infections
- you will reduce the risk of sudden infant death syndrome (SIDS), also known as “cot death”.
Help to quit smoking
Information and advice to help you stop smoking.
Local stop smoking services are free, friendly and can massively boost your chances of quitting for good.
These services staffed by expert advisers provide a range of proven methods to help you quit.
They’ll give you accurate information and advice, as well as professional support, during the first few months you stop smoking.
How to contact a stop smoking adviser
Your GP, pharmacist or health visitor can refer you, or you can phone your local stop smoking service to make an appointment with an adviser.
In England
Find stop smoking services in England
Call the free Smokefree National Helpline on 0300 123 1044
They also make it easy and affordable for you to get stop smoking treatments, such as:
- Bupropion (Zyban)
- nicotine replacement therapy, such as patches and gum
111: Guidance & Information
NHS 111 can help if you think you need medical help right now.
They can direct you to the best place to get help if you cannot contact your GP during the day, or when your GP is closed (out-of-hours).
The 111 Service
What is the 111 service?
NHS 111 is here to make it easier and quicker for patients to get the right advice or treatment they need, be that for their physical or mental health.
The service is available to you 24 hours a day, 7 days a week.
Help from NHS 111 is FREE, you can:
- Go online to 111.nhs.uk (for assessment of people aged 5 and over only).
- Call 111 for free from a landline or mobile phone.
This section covers everything about the 111 service, including how to find and register with a local GP and how to book an appointment.
About 111
NHS 111 helps people get the right advice and treatment when they urgently need it.
Clinicians, such as nurses, doctors, pharmacists and paramedics now play an important role in NHS 111. In fact, over 50% of people who call 111 speak to someone in one of these roles.
In many cases NHS 111 clinicians and call advisors can give patients the advice they need without using another service such as their GP or A&E.
If needed, NHS 111 can book patients in to be seen at their local A&E / emergency department or an urgent treatment centre, emergency dental services, pharmacy or another more appropriate local service – as well as send an ambulance should the patient’s condition be serious or life-threatening.
NHS 111 is here to make it easier and quicker for patients to get the right advice or treatment they need, be that for their physical or mental health.
24 hours a day, 7 days a week.
To get help from NHS 111, you can:
- Go online to nhs.uk (for assessment of people aged 5 and over only).
- Call 111 for free from a landline or mobile phone.
- Alternative access to NHS 111
If you have difficulties communicating or hearing, you can:
- Call 18001 111 using the Relay UK app on your smartphone, tablet or computer, or via a traditional textphone; or
- Use the NHS 111 British Sign Language (BSL) interpreter service if you’re deaf and want to use the phone service.
NHS England has produced this video to help people with a learning disability, autism or both, to use the NHS 111 service.
Other resources are also available on the NHS 111 service including:
- a large print guide to NHS 111
- an easy read guide to NHS 111
- an audio guide to NHS 111
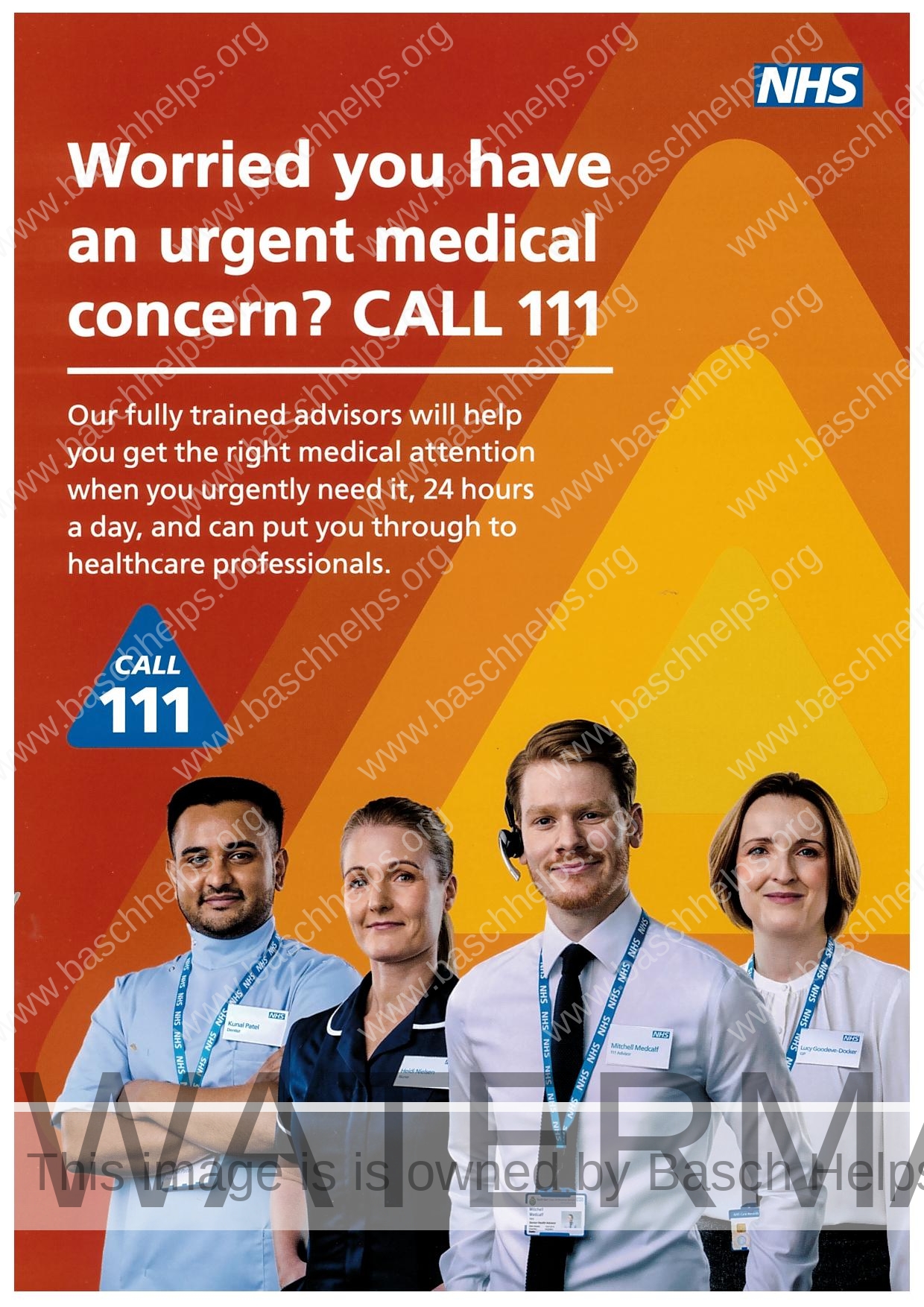
When to call 111
They can direct you to the best place to get help if you cannot contact your GP during the day, or when your GP is closed (out-of-hours).
Call 111 to speak to someone if you need to:
- discuss complex medical problems
- discuss worries about a long-term condition
- get end-of-life care, or report a death
- report child protection or vulnerable adult concerns
Other ways to contact 111 if you have a hearing problem or need help in other languages
Depending on what you need, you might be advised to:
- call 999 or go to A&E in an emergency
- go to an urgent treatment centre
- see an evening and weekend GP (out-of-hours GP)
- get a callback from a nurse
- contact an emergency dentist or find a dentist
- contact your own GP surgery
- see a pharmacist for a minor illness or to get medicine
- look after yourself safely at home
What happens during your call
When you call NHS 111, you will be asked:
- who you are
- where you’re calling from
- why you’re calling
- if it’s about you or someone else
If it’s about someone else, it’s better to call when you’re with the person so you can ask them to describe their symptoms.
Based on your answers, the health adviser will:
- send an ambulance for you if you need one
- refer you to an urgent care service
- refer you to another healthcare professional (such as a GP or dentist)
- arrange for you to visit an evening and weekend (out-of-hours) service
- arrange for a nurse to call you back
- give you self-care advice to follow at home
111 Online
Get help for your symptoms online
If you think you need medical help right now, 111 online can tell you what to do next.
It’s a digital triage service, available in England only, for people aged 5 and over.
What does triage mean? ‘Triage’ means answering a series of questions to check how ill you might be and what help you need.
Triage services do not give you a diagnosis. The more questions you are asked the less serious it’s likely to be.
They use the same triage system (‘algorithm’) as the 111 phone service, called NHS Pathways.
They ask for your location at the start so we can find services close to you that can help.
You don’t need to tell them who you are to use 111 online, but if they refer you to another service they will need some personal details from you.
111 online has about 120 topics to choose from, covering most common symptoms.
We ask questions about symptoms. We cannot give advice about conditions you already know you have.
The system can only triage one symptom at a time. If you have multiple symptoms, it is important to pick the one that is bothering you most.
Based on your answers to triage questions, we tell you what to do next. We rely on the NHS Directory of Services to show you the right place to get care in your area.

Use 111 Online Now
Get help for your symptoms online
If you think you need medical help right now, 111 online can tell you what to do next.
It’s simple, user friendly and will advise you on what action to take once you have completed a series of questions about your symptoms similar to if you were experience a face to face triage with a nurse at A & E.
When to dial 999: Guidance & Information
You should call 999 in a life-threatening emergency only. Life-threatening emergencies are different for adults and children.
When to call 999
At some point, most people will either witness or be involved in an accident, or experience a medical or mental health emergency.
Knowing what to do next and who to call can potentially save lives.
Call 999 in a medical or mental health emergency. This is when someone is seriously ill or injured and their life is at risk.
These emergencies can include:
- loss of consciousness
- a sudden confused state
- fits that are not stopping
- chest pain
- breathing difficulties
- severe bleeding that cannot be stopped
- severe allergic reactions (anaphylaxis)
- severe burns or scalds
- someone has seriously injured themselves or taken an overdose
Call 999 immediately if you think you or someone else is having a heart attack or stroke. Every second counts with these conditions.
Also call 999 if you think someone has had a major trauma, such as after a serious road traffic accident, a stabbing, a shooting, a fall from height, or a serious head injury.
What happens during a 999 call
1. Answer the questions
Once you’re connected to a call handler, you’ll have to answer a series of questions to establish what’s wrong, such as:
- where are you (including the area or postcode)?
- what phone number are you calling from?
- what has happened?
This will allow the operator to determine the most appropriate response as quickly as possible.
Dialling 999 does not necessarily mean an ambulance will be dispatched. The call handler will decide what’s appropriate.
It may be safe enough for you to be seen elsewhere, or you can be given telephone advice by a medically trained clinical adviser.
An ambulance will be sent if it’s a life-threatening emergency.
Response units that could be dispatched include:
- an emergency ambulance
- a rapid response vehicle or motorbike
- a cycle response unit
- a community first responder
- a combination of the above
2. Do not hang up yet
Wait for a response from the ambulance control room. They might have further questions for you, such as:
- what’s the age, gender and medical history of the patient?
- is the person awake or conscious and breathing?
- is there any serious bleeding or chest pain?
- what is the injury and how did it happen?
The person handling your call will let you know when they have all the information they need.
You might also be given instructions about how to give first aid until the ambulance arrives.
Urgent Treatment Centre (UTC): Guidance & Information (London)
Urgent treatment centres provide medical help when it’s not a life-threatening emergency. They can diagnose and deal with many of the common problems people go to A&E for.
Urgent Treatment Centre
What is an Urgent Treatment Centre? Urgent treatment centres (UTCs) are GP-led, open at least 12 hours a day, every day, offer appointments that can be booked through 111 or through a GP referral, and are equipped to diagnose and deal with many of the most common ailments people attend A&E for.
Find your nearest Urgent Treatment Centre using this link –
https://www.nhs.uk/Service-Search/other-services/Urgent%20Care/LocationSearch/1824
When to visit a UTC
You can go to an urgent treatment centre (UTC)
If you need urgent medical attention, but it’s not a life-threatening situation. UTCs are open at least 12 hours a day, every day.
Conditions that can be treated at an urgent treatment centre include:
- sprains and strains
- suspected broken limbs
- minor head injuries
- cuts and grazes
- bites and stings
- minor scalds and burns
- ear and throat infections
- skin infections and rashes
- eye problems
- coughs and colds
- high temperature in child and adults
- stomach pain
- being sick (vomiting) and diarrhoea
- emergency contraception
Accident & Emergency (A&E): Guidance & Information (London)
A&E (accident and emergency) is for serious injuries and life-threatening emergencies only. It is also known as the emergency department or casualty.
Life-threatening emergencies are different for adults and children.
This comprehensive guide provides information on what the accident & emergency department does, how it responds to different illnesses & injury and where to find your local Accident & Emergency Department.
Accident & Emergency
A&E departments offer access 24 hours a day, 365 days a year.
A&E staff includes emergency medicine doctors, nurses, diagnostic radiographers, reception staff, porters and healthcare assistants. Medical staff are highly trained in all aspects of emergency medicine.
An A&E department (also known as emergency department or casualty) deals with genuine life-threatening emergencies, such as:
- loss of consciousness
- a sudden confused state
- fits that are not stopping
- chest pain
- breathing difficulties
- severe bleeding that cannot be stopped
- severe allergic reactions (anaphylaxis)
- severe burns or scalds
- stroke
- major trauma such as a road traffic collision
- feelings of self-harm or suicide


Find your nearest A & E Department
Not all hospitals have an A&E department.
Find your nearest A&E
Many hospitals have their own website and may describe the urgent and emergency care services they offer.

What happens at A & E
If you arrive by ambulance, the ambulance crew will provide the relevant details to reception and hand you over to the clinical staff. If you’re seriously ill, the staff may already know because the ambulance crew will usually alert them.
If you’re not in a life-threatening or serious condition, you’ll be prioritised by the A&E hospital team along with other patients waiting to be seen – arriving by ambulance does not necessarily mean you’ll be seen sooner than if you had walked in to A&E.
If you go to A&E by yourself, you’ll need to register when you arrive. You’ll be asked a few questions such as name and address but also why you’re visiting A&E. If you’ve been to the hospital before, the reception staff will also have access to your health records.
Once you’ve registered, you’ll be asked to wait until you’re called for your assessment.
Some hospitals have a separate children’s A&E department where medical staff are specially trained to deal with children’s health issues. You may be asked to go straight to the children’s area where your child can be registered and assessed
If you need special assistance because of a physical or mental disability then you should let staff know right away. The hospital may be able to call a Learning Disabilities Liaison, a member of their liaison psychiatry team, or provide any other assistance you or your carer may need.

Assessment & Outcome
Once you’ve registered you’ll generally be pre-assessed by a nurse or doctor before further actions are taken. This is called triage. The process is carried out on all patients attending A&E. Triage ensures people with the most serious conditions are seen first.
What happens next depends on the results of your assessment. Sometimes further tests need to be arranged before a course of action can be decided.
If your situation is more complicated, you may be seen by an A&E doctor or referred to a specialist unit. For example, this could happen for eye injuries, strokes or emergency gynaecology.

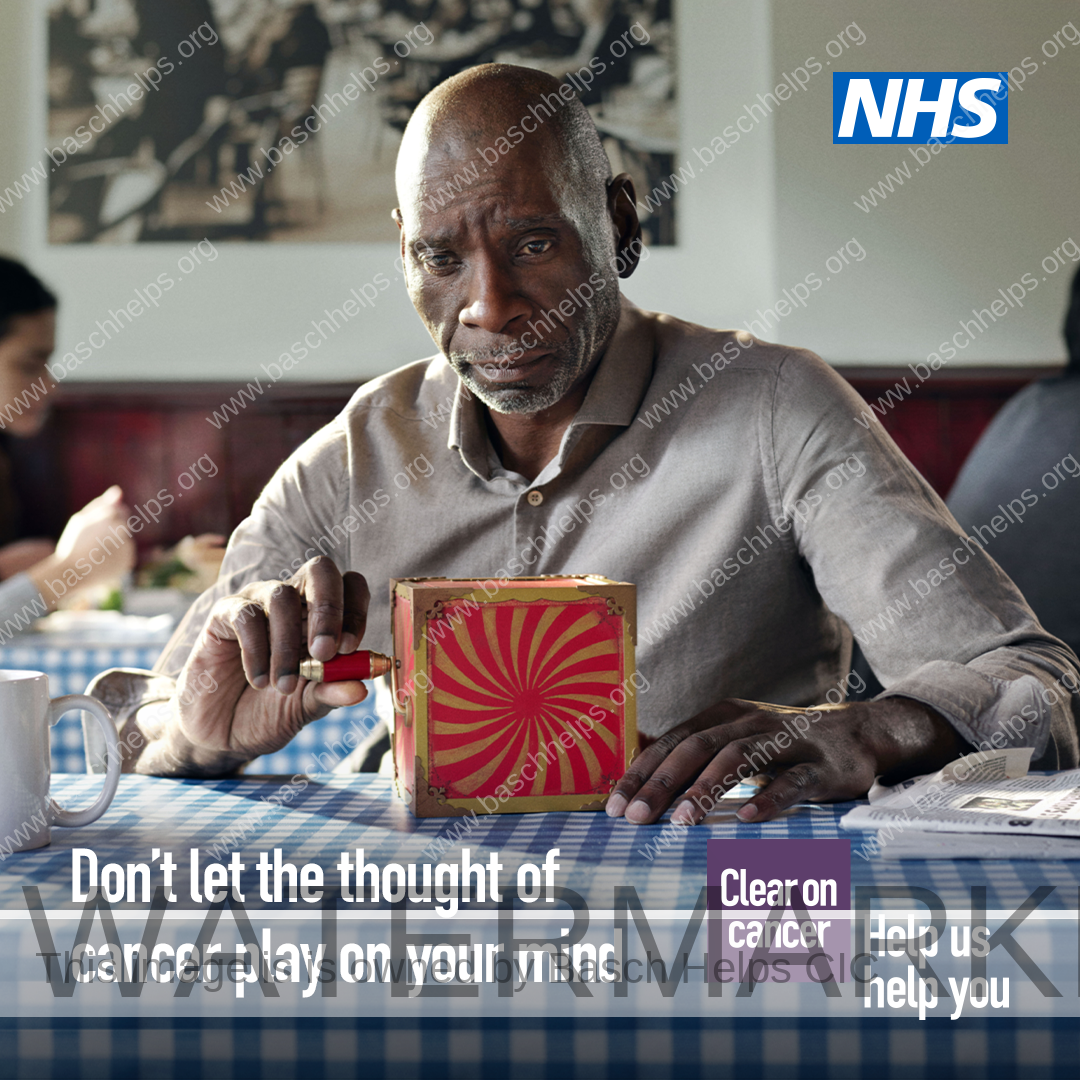
Cancer Screening Services: Guidance & Information
NHS cancer screening programmes can help to diagnose cancer or risk of cancer earlier and improve the likelihood of successful treatment. There are three national cancer screening programmes in England.
NHS Cancer Screening
NHS cancer screening programmes can help to diagnose cancer or risk of cancer earlier and improve the likelihood of successful treatment. There are three national cancer screening programmes in England.
If you are eligible, please make every effort to have your screening test. Screening tests can detect a problem early, before you have any symptoms. Finding out about a problem early can mean that treatment is more effective.
About 1 in 8 women in the UK are diagnosed with breast cancer during their lifetime. If it’s detected early, treatment is more successful and there’s a good chance of recovery.
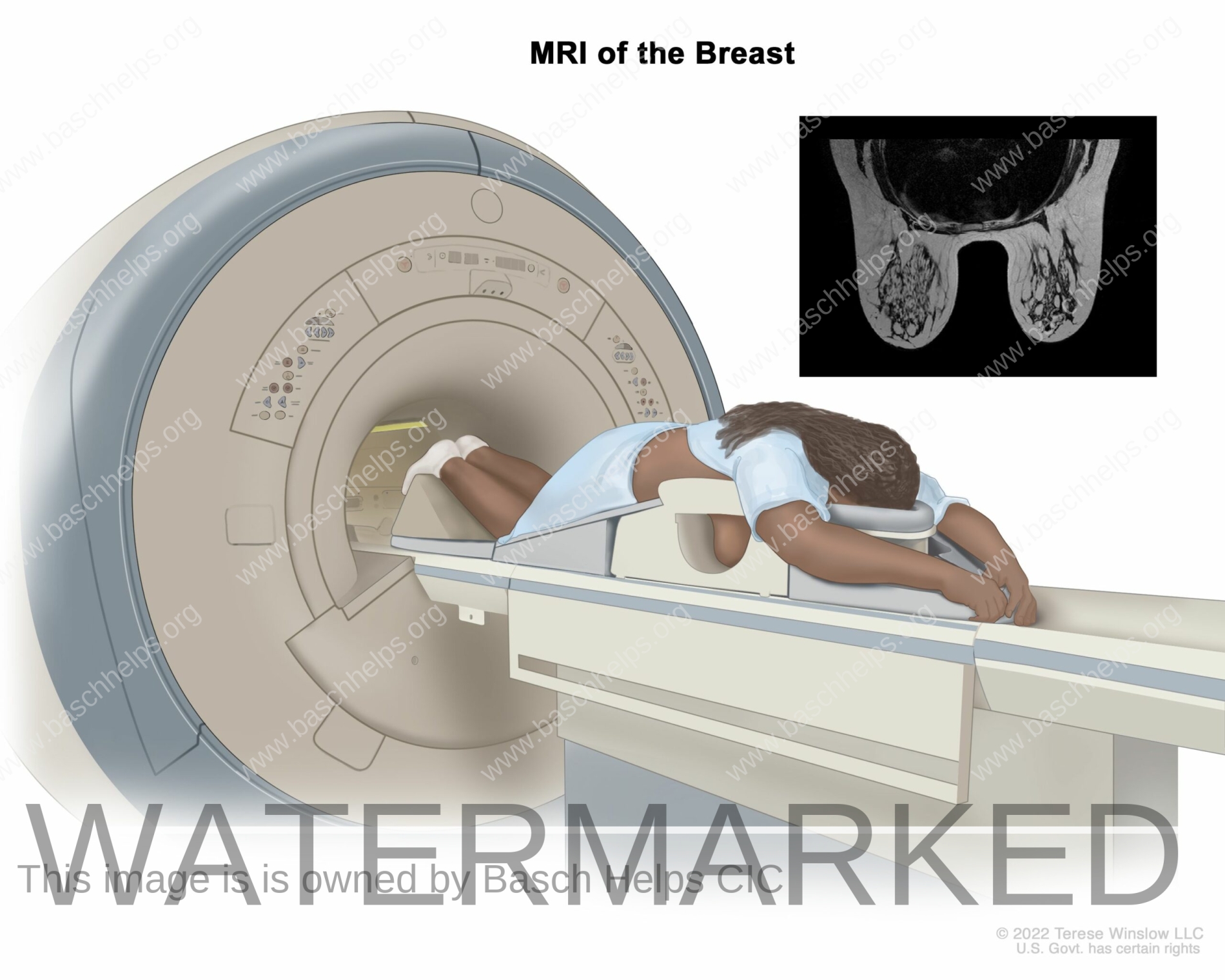
Breast screening uses an X-ray test called a mammogram that can spot cancers when they’re too small to see or feel.
Breast screening is offered to women aged 50 to their 71st birthday in England. You’ll first be invited for screening within three years of your 50th birthday
There is also currently a trial to examine the effectiveness of offering some women one extra screen between the ages of 47 and 49, and one between the ages of 71 and 73.
You may be eligible for breast screening before the age of 50 if you have a very high risk of developing breast cancer.
If you are 71 or over, you will stop receiving screening invitations. You can still have screening once you are 71 or over if you want to and can arrange an appointment by contacting your local screening unit.
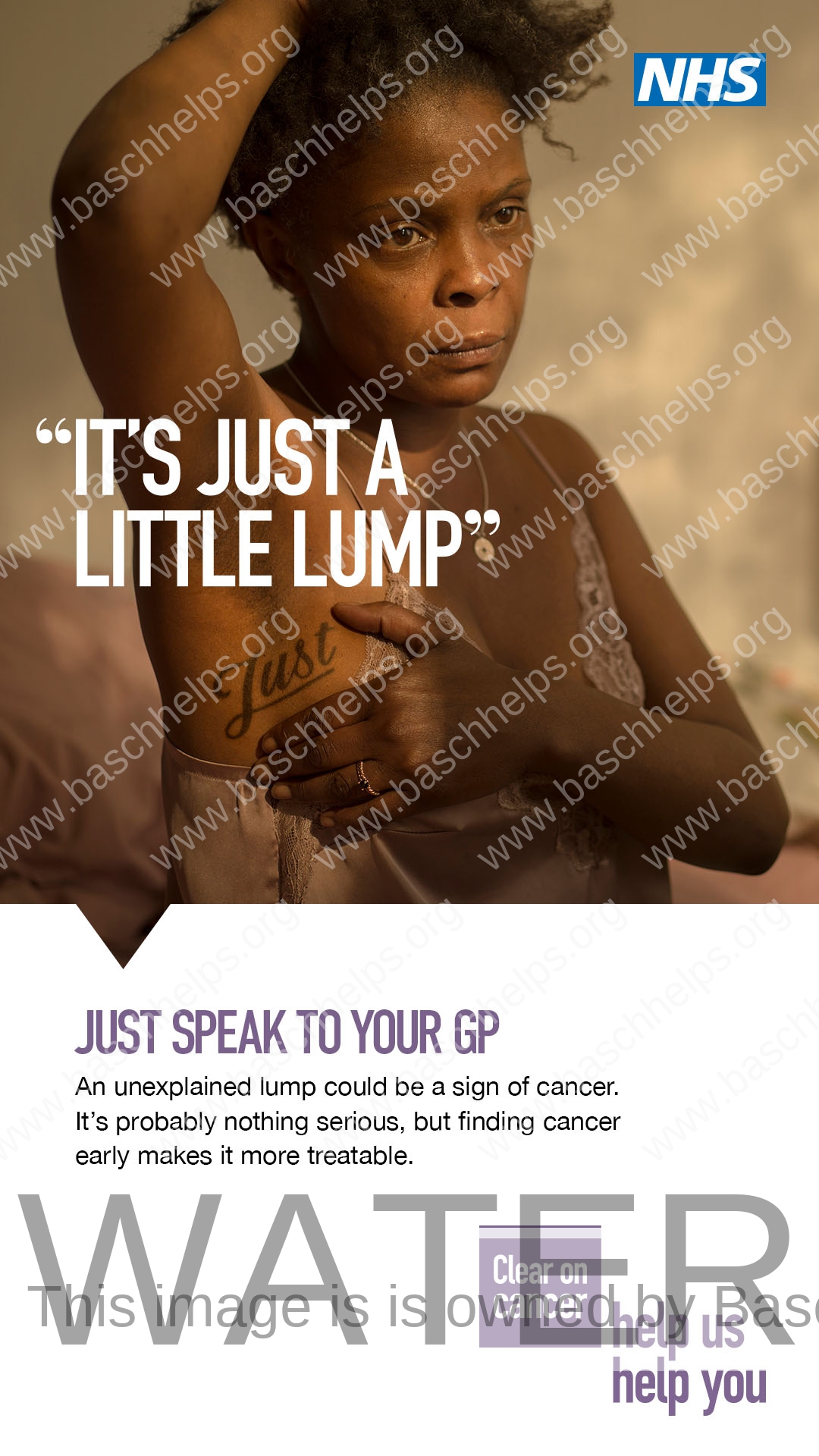
If you’re worried about breast cancer symptoms, such as a lump or an area of thickened tissue in a breast, or you notice that your breasts look or feel different from what’s normal for you, do not wait to be offered screening. See a GP.
The NHS cervical screening programme in England is offered to people with a cervix aged from 25 to 64. Routine screening is offered every three years up to 49 years of age and every five years from 50 to 64 years of age. Depending on the result of the screen, people may be recalled earlier than these routine intervals.
As part of the NHS Cervical Screening Programme, all samples taken at cervical screening appointments are now being tested for high risk Human Papillomavirus (HPV) in the first instance. This is the virus which causes nearly all cervical cancers. Samples that test positive for HPV will then go on to be further analysed with Liquid Based Cytology to detect cell abnormalities. The new test will identify more people at risk of cervical cancer earlier and could prevent around 600 additional cancers a year.
HPV is a very common virus which effects around 8 in 10 people; it is nothing to be embarrassed about, and in many cases, your immune system will naturally get rid of HPV.
For more information on the cervical screening programme, please visit the NHS cervical screening pages. Alternatively, visit the gov.uk website or Jo’s Cervical Cancer Trust’s website.

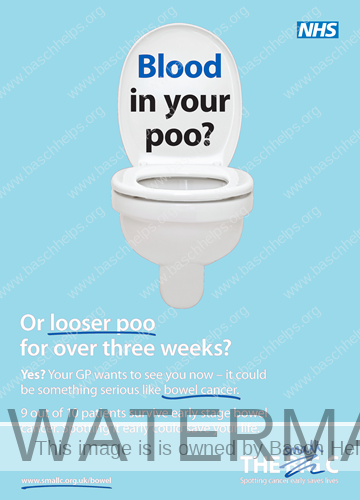
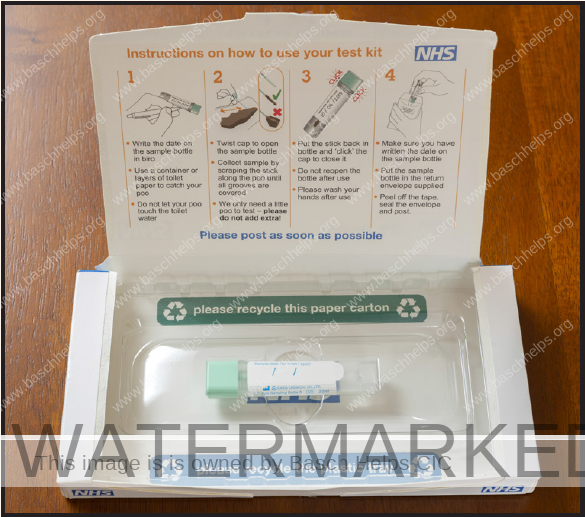
Bowel cancer survival is improving and has more than doubled in the last 40 years in the UK. If diagnosed early, more than 90% of bowel cancer cases can be treated successfully.
Screening programmes test to see if people show any early signs of cancer. By detecting bowel cancer at an early stage, treatment has a better chance of working.
As part of the NHS Bowel Cancer Screening Programme, men and women aged 60-74 are sent a home testing kit every two years to collect a small sample of poo to be checked for tiny amounts of blood which could be caused by cancer. In 2019, the home testing kit was changed from the guaiac Faecal Occult Blood Test (gFOBT) to the Faecal Immunochemical Test (FIT) because it is:
- more accurate – it can detect smaller signs of blood hidden in poo samples, which can be an early sign of bowel cancer.
- easier to use – only one sample is required. The gFOBt required three samples to be taken on three different days.
As part of the NHS Long Term Plan, there is also a commitment to lower the bowel screening age to 50 and improve the sensitivity of the screening test further. With support from Public Health England and Health Education England, the NHS is working on plans to safely implement these significant changes, which will include needing extra staff to be trained to undertake extra colonoscopies and other investigations.
For more information on the bowel cancer screening test, please visit the nhs.uk bowel cancer screening pages. You can also find information on the signs and symptoms of bowel cancer on the nhs.uk website.
Breast Cancer Awareness
Breast Cancer
Breast cancer is the most common type of cancer in the UK. Most women diagnosed with breast cancer are over the age of 50, but younger women can also get breast cancer.
For this reason, it’s vital that women check their breasts regularly for any changes and always have any changes examined by a GP.
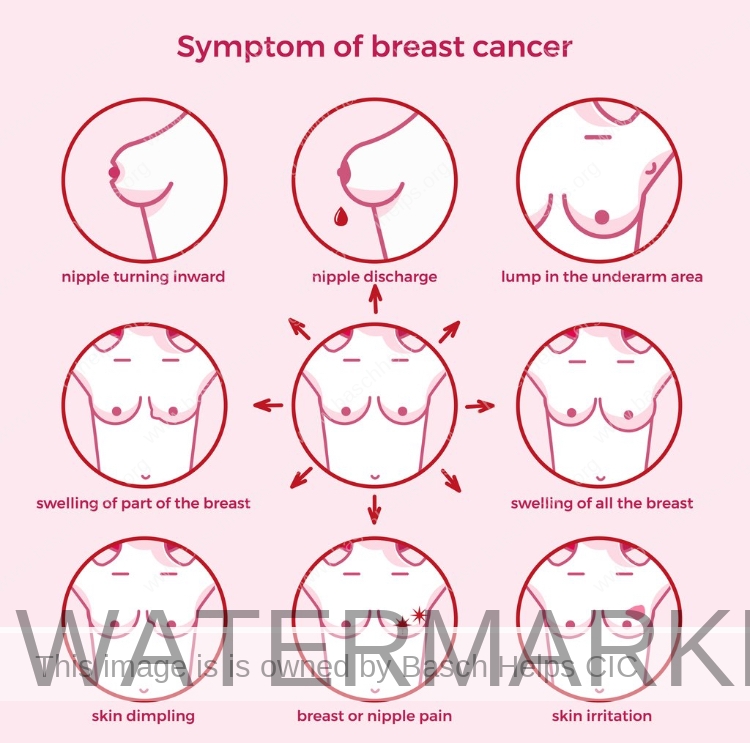
Symptoms of Breast Cancer
Breast cancer can have several symptoms, but the first noticeable symptom is usually a lump or area of thickened breast tissue.
Most breast lumps are not cancerous, but it’s always best to have them checked by a doctor.
You should also see a GP if you notice any of these symptoms:
- a change in the size or shape of one or both breasts
- discharge from either of your nipples, which may be streaked with blood
- a lump or swelling in either of your armpits
- dimpling on the skin of your breasts
- a rash on or around your nipple
- a change in the appearance of your nipple, such as becoming sunken into your breast
Breast pain is not usually a symptom of breast cancer.
Find out more about the symptoms of breast cancer.
Causes of breast cancer
The exact causes of breast cancer are not fully understood. However, there are certain factors known to increase the risk of breast cancer.
These include:
- age – the risk increases as you get older
- a family history of breast cancer
- a previous diagnosis of breast cancer
- a previous non-cancerous (benign) breast lump
- being tall, overweight or obese
- drinking alcohol
Find out more about the causes of breast cancer.


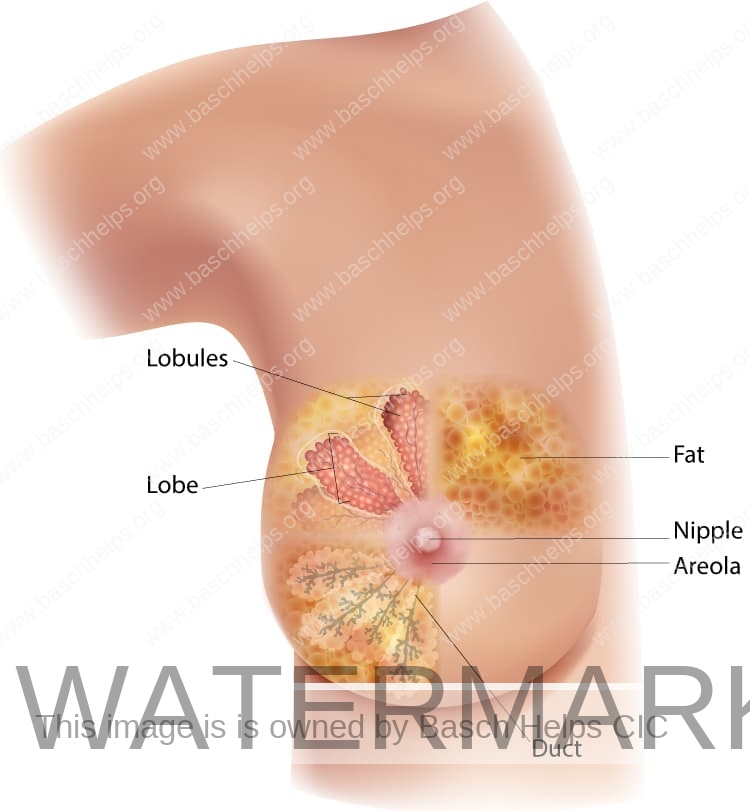
Diagnosing & screening breast cancer
Mammographic screening, where X-ray images of the breast are taken, is the most commonly available way of finding a change in your breast tissue (lesion) at an early stage.
However, you should be aware that a mammogram might fail to detect some breast cancers.
It might also increase your chances of having extra tests and interventions, including surgery, even if you’re not affected by breast cancer.
Women with a higher-than-average risk of developing breast cancer may be offered screening and genetic testing for the condition.
As the risk of breast cancer increases with age, all women who are 50 to 70 years old are invited for breast cancer screening every 3 years.
Women over the age of 70 are also entitled to screening and can arrange an appointment through their GP or local screening unit.
The NHS is in the process of extending the programme as a trial, offering screening to some women aged 47 to 73.
Find out more about breast cancer screening.
Treating breast cancer
If cancer is detected at an early stage, it can be treated before it spreads to other parts of the body.
Breast cancer is treated using a combination of:
- surgery
- chemotherapy
- radiotherapy
Surgery is usually the first type of treatment you’ll have, followed by chemotherapy or radiotherapy or, in some cases, hormone or targeted treatments.
The type of surgery and the treatment you have afterwards will depend on the type of breast cancer you have. Your doctor should discuss the best treatment plan with you.
In a small proportion of women, breast cancer is discovered after it’s spread to other parts of the body (metastatic breast cancer).
Secondary cancer, also called advanced or metastatic cancer, is not curable, so the aim of treatment is to relieve symptoms.
Find out more about treating breast cancer.


Cervical Cancer Awareness
Cervical Cancer
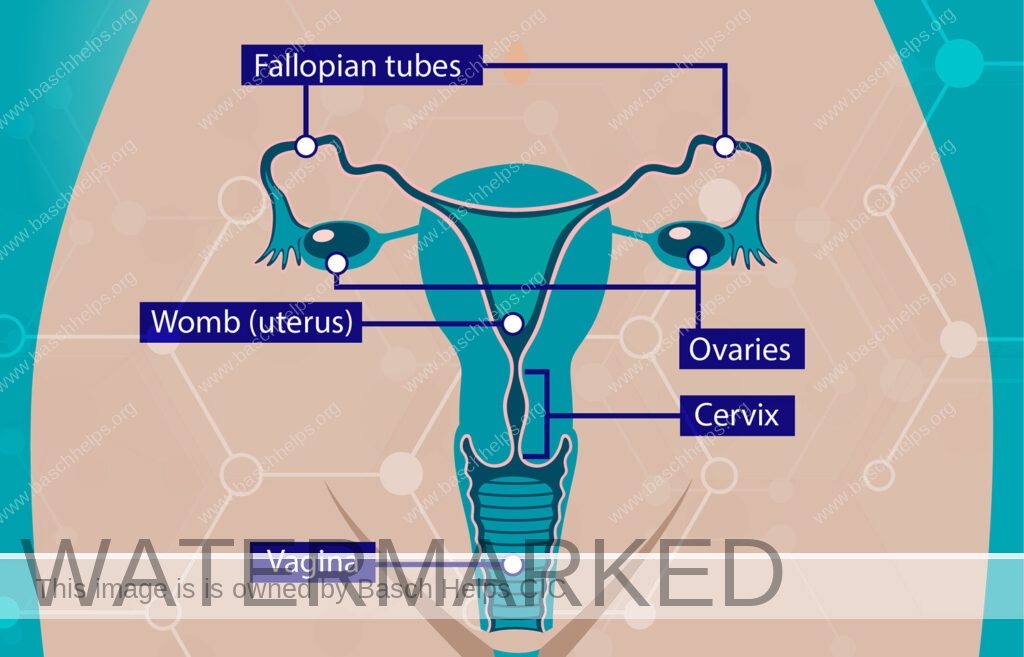
Cervical cancer is a cancer that’s found anywhere in the cervix. The cervix is the opening between the vagina and the womb (uterus). It’s part of the reproductive system and is sometimes called the neck of the womb.
Nearly all cervical cancers are caused by an infection from certain types of human papillomavirus (HPV).
It can often be prevented by attending cervical screening, which aims to find and treat changes to cells before they turn into cancer. Cervical cancer usually grows very slowly. How serious it is depends on how big it is, if it has spread and your general health.
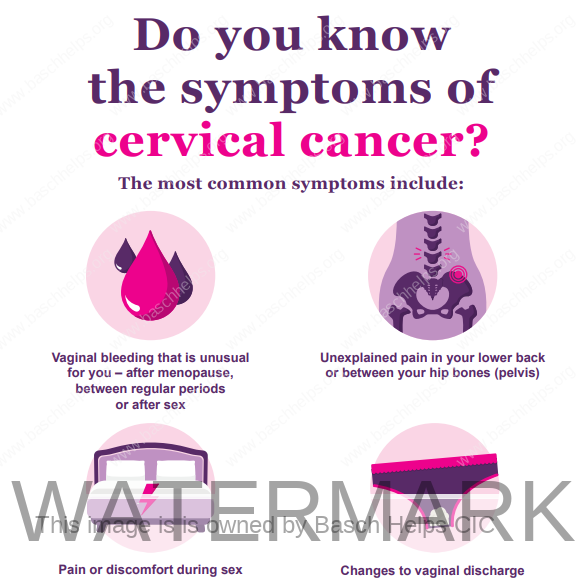
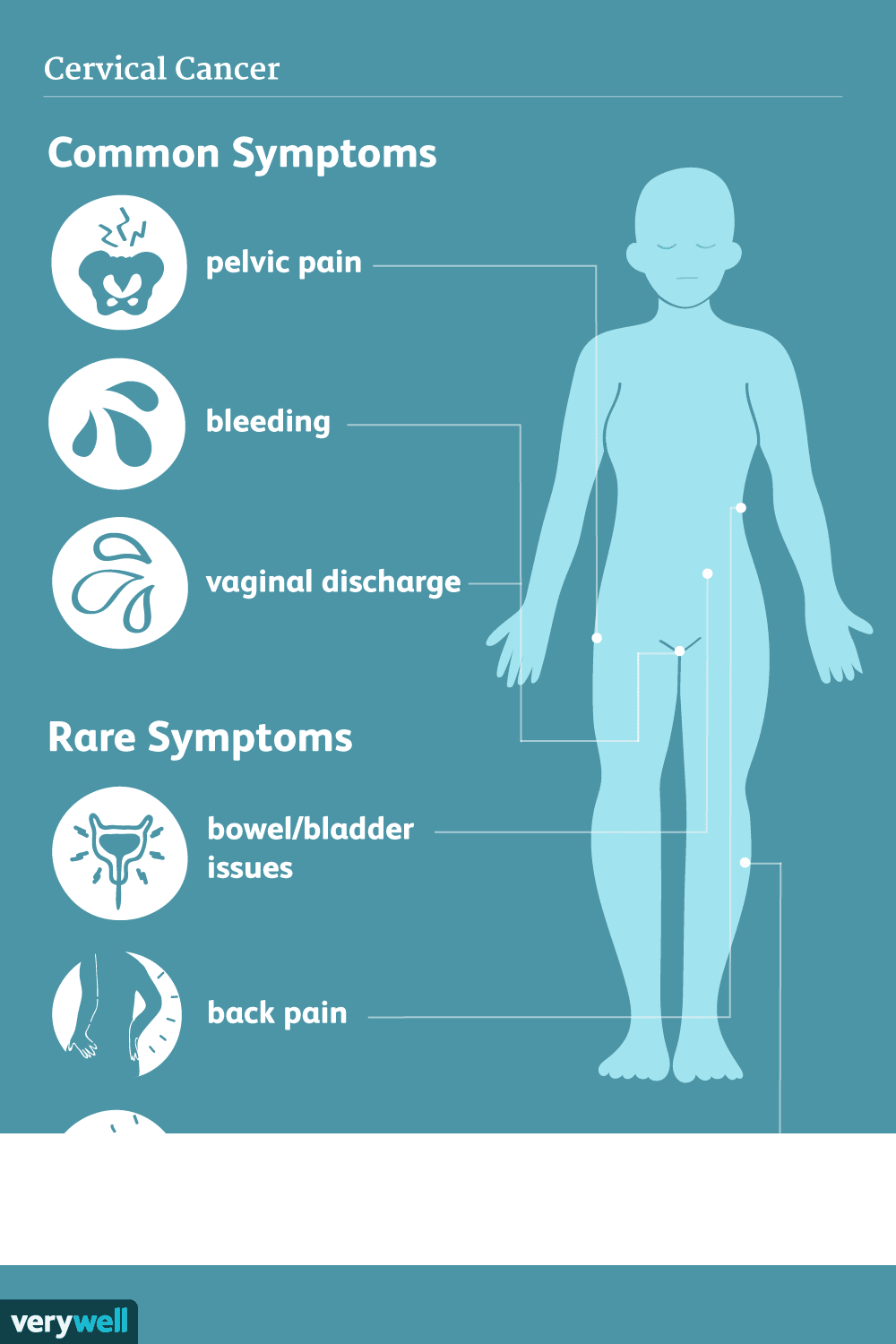
Symptoms of Cervical Cancer
Symptoms of cervical cancer include:
- vaginal bleeding that’s unusual for you – including bleeding during or after sex, between your periods or after the menopause, or having heavier periods than usual
- changes to your vaginal discharge
- pain during sex
- pain in your lower back, between your hip bones (pelvis), or in your lower tummy
If you have another condition like fibroids or endometriosis, you may get symptoms like these regularly.
You might find you get used to them. But it’s important to be checked by a GP if your symptoms change, get worse, or do not feel normal for you.
Causes of cervical cancer
Main causes of cervical cancer
Nearly all cervical cancers are caused by an infection with certain high-risk types of human papillomavirus (HPV).
You can get HPV from:
- any skin-to-skin contact of the genital area
- vaginal, anal or oral sex
- sharing sex toys
Who is more likely to get cervical cancer
Anyone with a cervix can get cervical cancer. This includes women, trans men, non-binary people, and intersex people with a cervix.
You cannot get cervical cancer if you’ve had surgery to remove your womb and cervix (total hysterectomy).
You might also be more likely to get cervical cancer if:
- you’re under 45 – cervical cancer is more common in younger people
- you have a weakened immune system, like if you have HIV or AIDS
- you have given birth to multiple children or had children at an early age (under 17 years old)
- your mother took the hormonal medicine diethylstilbestrol (DES) while pregnant with you – your GP can discuss these risks with you
- you’ve had vaginal, vulval, kidney or bladder cancer in the past
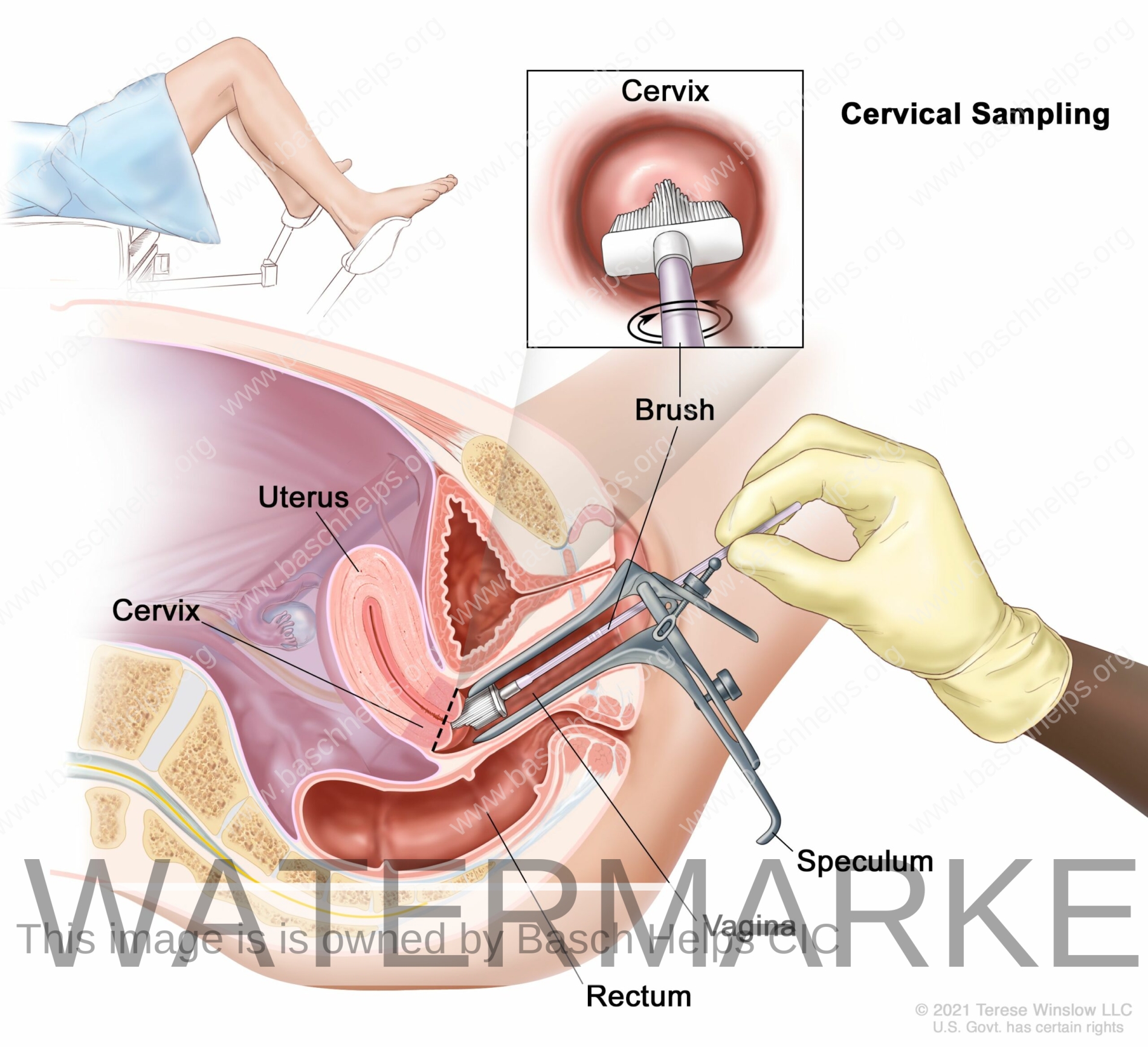
Diagnosing & screening cervical cancer
The GP may ask to examine you.
You can ask for a female doctor when you book your appointment.
You’ll be asked to undress from the waist down, behind a screen. You’ll be given a sheet to put over you.
If you have abnormal cells in your cervix, which could mean you have cervical cancer, you’ll usually be referred for a test to have a closer look at your cervix. This is called a colposcopy.
You’ll be asked to undress from the waist down, behind a screen. You’ll be given a sheet to put over you.
Treating cervical cancer
Being told you have cervical cancer can feel overwhelming. You may be feeling anxious about what will happen next.
It can help to bring someone with you to any appointments you have.
A group of specialists will look after you throughout your diagnosis, treatment and beyond.
This will include a clinical nurse specialist, who will be your main point of contact during and after treatment.
Cervical cancer is often treatable.
The treatment you have will depend on:
- the size and type of cervical cancer you have
- where the cancer is
- if it has spread
- your general health
It will usually include surgery, chemotherapy or radiotherapy. It may also include treatment with targeted medicines to treat the cancer.
The specialist care team looking after you will:
- explain the treatments, benefits and side effects
- work with you to create a treatment plan that’s best for you
- talk to you about the impact that treatment may have on your fertility

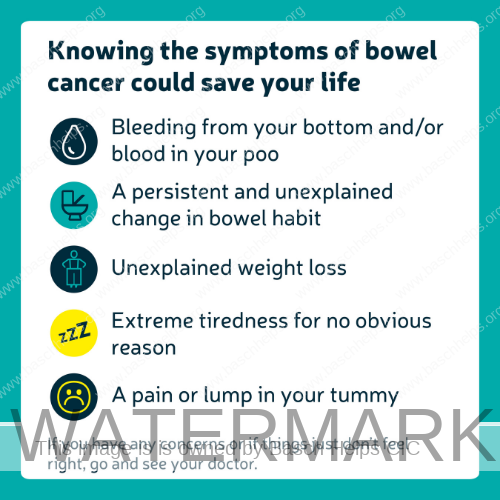
Bowel Cancer Awareness
Bowel Cancer
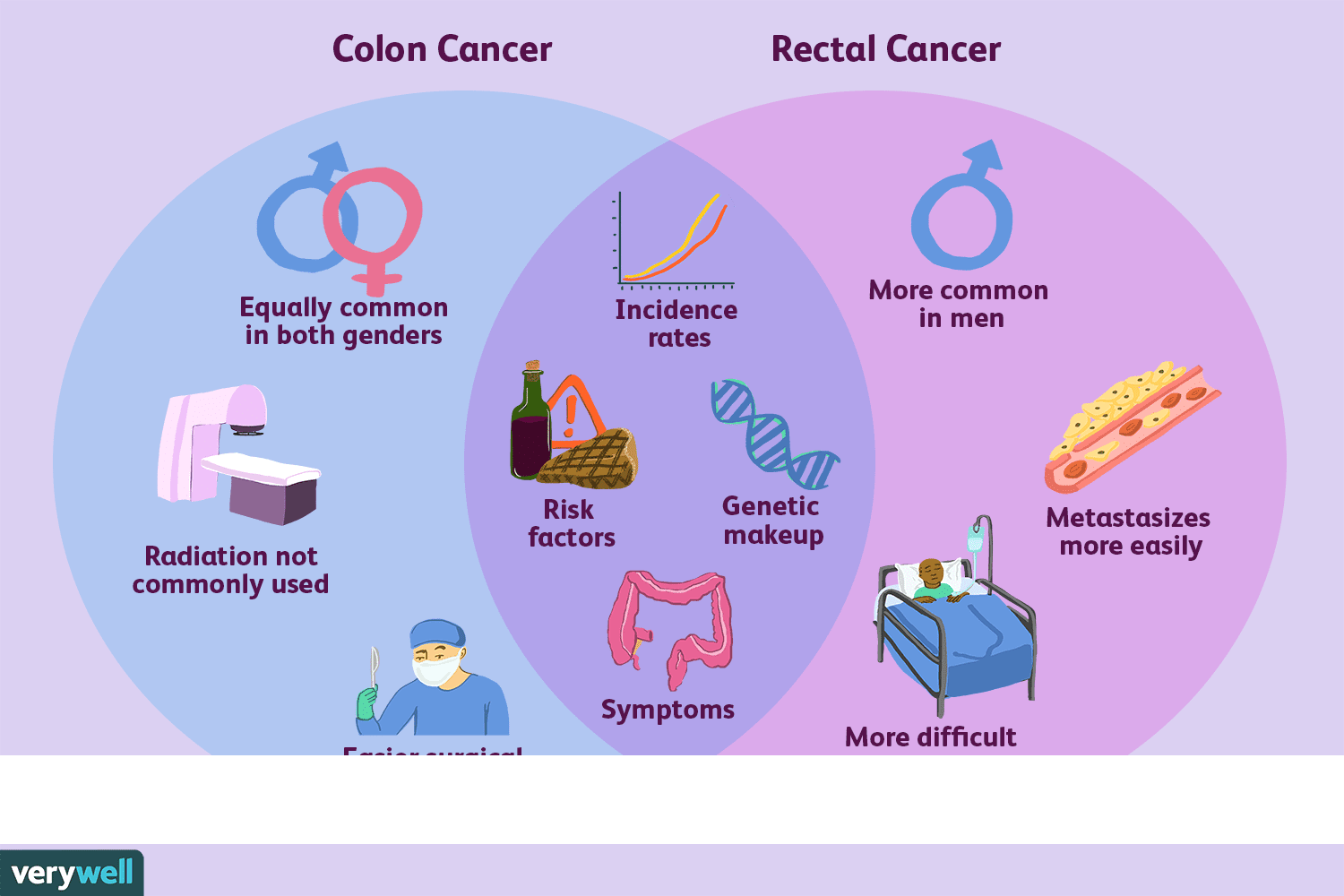
Bowel cancer is cancer found anywhere in the large bowel, which includes the colon and rectum. It’s one of the most common types of cancer in the UK.
- Bowel cancer is cancer that’s found anywhere in the large bowel, which includes the colon and rectum.
- The large bowel is part of your digestive system. It helps absorb water from your food and removes food waste from your body.
- How serious bowel cancer is depends on how big the cancer is, if the cancer has spread, and your general health.
- Bowel cancer is one of the most common types of cancer in the UK.
- Bowel cancer screening can pick up bowel cancer early, which may mean it’s easier to treat.

Symptoms of Bowel Cancer
Symptoms of bowel cancer may include:
- changes in your poo, such as having softer poo, diarrhoea or constipation that is not usual for you
- needing to poo more or less often than usual for you
- blood in your poo, which may look red or black
- bleeding from your bottom
- often feeling like you need to poo, even if you’ve just been to the toilet
- tummy pain
- bloating
- losing weight without trying
- feeling very tired for no reason
Causes of bowel cancer
It’s not always known what causes bowel cancer, but it can be caused by genetic changes, lifestyle, and environmental factors.
Having certain health conditions can also make you more likely to get bowel cancer.
You may be more likely to get bowel cancer if:
- you’re over 50
- you smoke
- you’re overweight
- a close relative has had bowel cancer
- you have inflammatory bowel disease, which includes Crohn’s disease and ulcerative colitis
- you have small growths in your bowel called bowel polyps
- you have Lynch Syndrome or familial adenomatous polyposis

Diagnosing & screening bowel cancer
The doctor will ask you more about your symptoms, general health, medical history, and if anyone in your family has had bowel cancer.
Depending on your symptoms, the doctor may feel your tummy and ask to do a rectal examination. This is where they put a gloved finger inside your bottom to check for any lumps.
You’ll be asked to undress from the waist down for the rectal exam. You can ask for a male or female doctor or nurse.
You can ask for someone else to be in the room with you when the rectal examination happens.
You may also be asked for a poo sample (stool sample) for testing.
If a GP refers you to a specialist because they think you could have bowel cancer, you’ll have tests to check for cancer.
The main test for bowel cancer is a colonoscopy. This is where a thin, flexible, tube with a camera is used to look inside your bowel.
It may be uncomfortable but it should not be painful. You’ll be offered a sedative and painkillers to help make you feel more comfortable.
During the colonoscopy, a small sample of the lining of your bowel may be taken for testing (called a biopsy)
Treating bowel cancer
The treatment you’ll have for bowel cancer depends on:
- the size of the cancer
- if the cancer is in your colon or rectum, or both
- if it has spread to other parts of your body
- if the cancer has certain genetic changes
- your age and general health
You may be offered a combination of treatments including surgery, chemotherapy, radiotherapy, and targeted medicines.
Your specialist treatment team will:
- explain the treatments, the benefits and side effects
- work with you to make a treatment plan that’s best for you
- help you to manage the side effects of treatment
If you have any questions or worries, you can talk to your specialist team.
Vaccinations for Adults: Guidance & Information (London Only)
Information and guidance about the available vaccinations through the NHS and your local pharmacies or GP.

Getting a flu jab
Flu vaccination is safe and effective. It’s offered every year through the NHS to help protect people at risk of getting seriously ill from flu.
Flu vaccination is important because, while flu is unpleasant for most people, it can be dangerous and even life threatening for some people, particularly those with certain health conditions.
The best time to have your flu vaccine is in the autumn or early winter before flu starts spreading. But you can get your vaccine later.
Who is eligible for a flu jab
The flu vaccine is given free on the NHS to adults who:
- are 50 and over (including those who will be 50 by 31 March 2023)
- have certain health conditions
- are pregnant
- are in long-stay residential care
- receive a carer’s allowance, or are the main carer for an older or disabled
- person who may be at risk if you get sick
- live with someone who is more likely to get a severe infection due to a weakened immune system, such as someone living with HIV, someone who has had a transplant, or is having certain treatments for cancer, lupus or rheumatoid arthritis

Children can get an immunity boost too
The children’s nasal spray flu vaccine is safe and effective. It’s offered every year to children to help protect them against flu.
This page is about flu vaccination for children. Find out about flu vaccination for adults.
Flu is caused by the influenza virus. It can be a very unpleasant illness for children. It can also lead to serious problems, such as bronchitis and pneumonia.
Children can catch and spread flu easily. Vaccinating them also protects others who are vulnerable to flu, such as babies and older people.
The nasal spray flu vaccine is free on the NHS for:
- children aged 2 or 3 years on 31 August 2022 (born between 1 September 2018 and 31 August 2020)
- all primary school children (Reception to Year 6)
- some secondary school aged children
- children aged 2 to 17 years with long-term health conditions
If your child is aged between 6 months and 2 years and has a long-term health condition that makes them at higher risk from flu, they’ll be offered a flu vaccine injection instead of the nasal spray.
Find out more:
https://www.nhs.uk/conditions/vaccinations/child-flu-vaccine/

Get your Covid Booster Jab
Everyone aged 5 (on or before 31 August 2022) and over can get a 1st and 2nd dose of the COVID-19 vaccine.
People aged 16 and over, and some children aged 12 to 15, can also get a booster dose.
You can also visit our dedicated Covid-19 Hub which has useful information on what the Covid virus is, understanding the different variants and advice about vaccination.
2022 © The logo, name, slogan and the word AngelBox™ are registered Trademarks of Basch Helps CIC. All Rights Reserved
Your Baby, Your Choice, Your AngelBox
London's Best Newborn Emergency Relief Provider





















































 At 8-16 weeks your baby should have taken all these vaccinations
It's important that vaccines are given on time for the best protection, but if you or your child missed a vaccine, contact your GP to catch up.
To get more information on how to book an appointment in London.
At 8-16 weeks your baby should have taken all these vaccinations
It's important that vaccines are given on time for the best protection, but if you or your child missed a vaccine, contact your GP to catch up.
To get more information on how to book an appointment in London.
